| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org/ |
Original Article
Volume 5, Number 2-3, September 2015, pages 165-170
Open Inguinal Hernia Repair Using Polypropylene Mesh: A Patient Reported Survey of Long-Term Outcomes
Philip Bagshawa, b, c, Suzanne Wellera, Carl Shawa, Christopher Framptonb
aCanterbury Charity Hospital Trust, PO Box 20409, Christchurch 8543, New Zealand
bUniversity of Otago - Christchurch, Christchurch School of Medicine, Riccarton Road, Christchurch, New Zealand
cCorresponding Author: Philip Bagshaw, Canterbury Charity Hospital Trust, PO Box 20409, Christchurch 8543, New Zealand
Manuscript accepted for publication August 19, 2015
Short title: Inguinal Hernia Repair Outcomes
doi: http://dx.doi.org/10.14740/jcs276w
| Abstract | ▴Top |
Background: Since 2005, volunteer surgeons at the Canterbury Charity Hospital have performed Lichtenstein inguinal herniorrhaphies, using traditional heavyweight Prolene mesh, on some patients who were refused treatment by the local district health board because of service rationing. Long-term results were assessed by a postal survey, using a previously published, patient-completed questionnaire.
Methods: During 2008 to 2013, inclusive, 214 herniorrhaphies were performed. Of these, 141/208 (67.8%) completed the questionnaire. This covered acute complications, chronic mesh inguinodynia syndrome symptoms, and hernia recurrences. No other sources of follow-up data were added.
Results: Of 141 participants, four had recurrent and seven bilateral hernias. Mean age was 60.27 years (range 21.64 - 83.99 years). Mean length of follow-up was 3.11 years (range 0.79 - 6.15 years). The 69/141 (48.9%) participants’ recording of local adverse responses comprised: abnormal touch sensation in 43/140 (30.7%); sensation of repair material under wound in 26/140 (18.6%); discomfort in 22/140 (15.7%); pain at rest, on movement or exercise in 16/139 (11.5%) to 5/140 (3.6%); related GP visits and sick leave in 7/141 (5.0%) and 3/141 (2.1%); analgesic requirement in 4/140 (2.9%); and no hernia recurrences.
Conclusions: The moderately high levels of mesh inguinodynia syndrome symptoms after Lichtenstein herniorrhaphy were similar to those reported elsewhere. They prompted us to change to the use of a lightweight Prolene mesh. The survey will be repeated to assess whether the change reduces the mesh inguinodynia syndrome symptom rate without affecting the hernia recurrence rate. Such surveys are potentially useful tools for long-term surgical outcomes assessment, particularly in areas where there are technical controversies.
Keywords: Outcome assessment (health care); Questionnaires; Self report; Hernia; Inguinal; Herniorrhaphy; Surgical mesh
| Introduction | ▴Top |
The Canterbury Charity Hospital (CCH) is run by a charitable trust. Since 2005, it has offered free day surgery to some patients in the Canterbury District Health Board (CDHB) region who: 1) have been turned down for treatment by the CDHB because of selective rationing of elective surgical services; 2) cannot afford private care; 3) do not qualify for Accident Corporation Compensation surgery funding; and 4) are medically fit for day surgery [1]. It is largely staffed by volunteers and solely funded by public charitable giving. Inguinal hernia repair is one of the most common reasons for patient referral.
Contemporary surgical operations for the repair of inguinal hernias use tension-free synthetic meshes to repair the defects in the inguinal canal. These meshes can be positioned by open surgery, such as the Lichtenstein operation, or by laparoscopic approaches. Both types of repair are now considered “gold standard” treatments [2].
Tension-free mesh repairs have much lower hernia recurrence rates than previous repair procedures, such as the Bassini operation, which closed the defects in the inguinal canal with sutures under tension [3]. The mesh repairs, however, have the disadvantage that some patients develop a constellation of post-operative local groin symptoms. These are somewhat subjectively divided into the categories of pain, the sensation of repair material under the wound, abnormal skin sensations (paraesthesia, hyperaesthesia, or hypoesthesia), and discomfort [4]. When these symptoms are present for more than 3 - 6 months after surgery, they have been termed the mesh inguinodynia syndrome (MIS) [5].
The Lichtenstein operation was chosen as the standard inguinal hernia repair procedure at the CCH. This decision was based on our volunteer surgical workforce’s greater experience with open surgery rather than with laparoscopic approaches, and because of the higher cost associated with the latter. The aim of the current survey was to assess the long-term clinical results of that decision, in terms of acute post-operative complications, MIS symptoms and hernia recurrences. A patient-completed questionnaire was used with the objectives of minimizing costs and impact on volunteer staff workload.
| Methods | ▴Top |
Patients with primary and recurrent inguinal hernias operated on at the CCH between January 1, 2008 and December 31, 2013 were included in the survey. Patients with bilateral hernias had the two sides repaired on separate occasions. Between August and September 2014, all patients were mailed: information about the survey; a request for written consent to participate; a previously published questionnaire [6] for them to complete; and a pre-paid, return-addressed envelope. Non-responders were sent a second mail request to participate 6 - 8 weeks later. The survey was approved by the New Zealand Southern Health and Disability Ethics Committee (August 6, 2014; Ethics ref: 14/STH/98).
Twelve senior, vocationally registered surgeons performed the operations, all of which were done under general anesthesia, with local anesthetic infiltration, antibiotic prophylaxis and intra-operative intermittent calf compression. The technique described by Lichtenstein and Shulman [7] was used and individually tailored traditional heavyweight Prolene mesh (80 - 85 g/m2 polypropylene; Johnson & Johnson, NZ Ltd) was employed for all cases and anchored in place with interrupted sutures of 2/0 Prolene (Johnson & Johnson, NZ Ltd). All patients were advised to return slowly to normal activities after 48 h, but to desist from driving a motor vehicle for 2 weeks, and to avoid all activities involving heavy lifting and violent straining for 6 weeks. All patients were offered a follow-up appointment at 2 weeks post-surgery.
The patient-reported questionnaire (questions A to P, listed in Table 1) asked about problems around the operative site, such as swelling in the groin or scrotum, changes in testicle size, pain, discomfort, abnormal skin sensation, restriction of activities, analgesic requirements, and other related issues. Responses were entered into a database; all inappropriate or equivocal responses were eliminated. No other sources of clinical outcome data were included.
 Click to view | Table 1. Yes Tick Box Responses to Questions (A to P) Posed in Survey Questionnaire |
Analyses were performed using SPSS V22.0. Fisher’s exact tests were used to compare questionnaire responses and Mann-Whitney U tests were used to compare follow-up times between the presence and absence of MIS symptoms. A two-tailed P ≤ 0.05 was considered significant. Where requested by participants, results of the survey will be sent to their GPs and outpatient review appointments will be offered.
| Results | ▴Top |
During the survey period, a total of 214 inguinal hernia repair operations were performed on adult patients at the CCH. Of these, data collection on five of the initial patients was incomplete and one patient was unable to give informed consent, so 208 patients were entered into the survey, and sent the relevant information and questionnaire (Fig. 1).
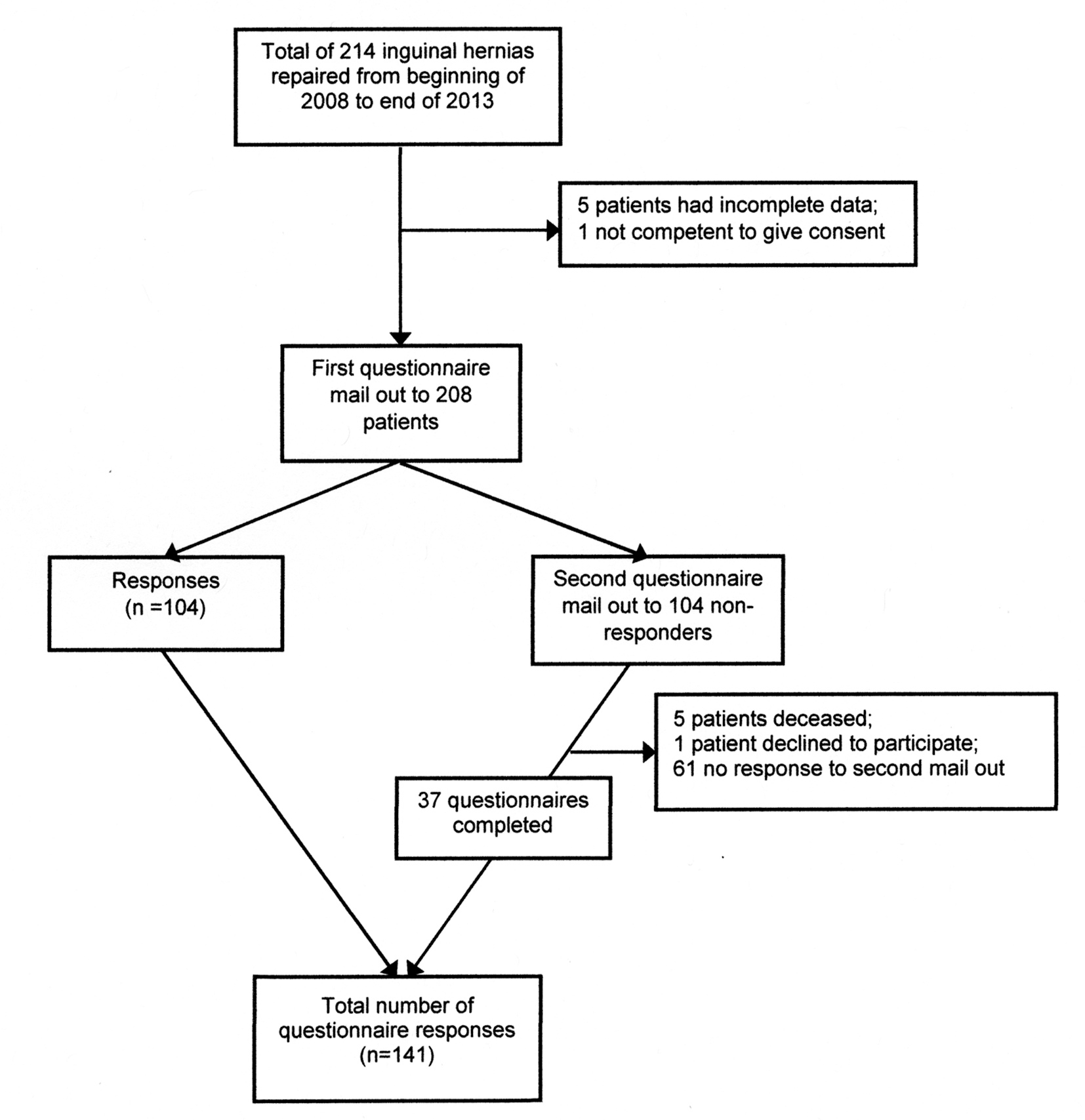 Click for large image | Figure 1. Flow diagram for the survey: responses to the two questionnaire mail outs. |
There were 104/208 (50.0%) responses with completed questionnaires to the first mail out. Postal addresses of the 104 non-responders were checked before the second mail out. Of these, 37 returned completed questionnaires, 67 did not respond, five were deceased, and one declined to participate. Therefore, when accrual was closed on December 10, 2014, there was a total of 141/208 (67.8%) completed responses. This comprised 131 (92.9%) males and 10 (7.1%) females with a mean age at operation of 60.27 years (SD = 13.91; minimum = 21.64 years; maximum = 83.99 years; n = 141); 68 (48.2%) right inguinal and 73 (51.8%) left inguinal hernia (four recurrent; seven bilateral). The survey was performed at a mean follow-up of 3.11 years (SD = 1.75; minimum = 0.79 years; maximum = 6.15 years; n = 141) per participant after hernia repair and represented a total of 438.17 participant-years of follow-up.
Participant-reported acute post-operative complications were: one reaction to codeine analgesia; one acute urinary retention requiring temporary catheterization; two wound hematomas and two small seromas that resolved spontaneously; five transient local wound swellings; and one suspected but unproven wound infection prescribed antibiotics.
Table 1 shows that adverse responses were: abnormal touch sensation in the inguinal area in 43 (30.7%) of participants; sensation of repair material under the wound in 26 (18.6%); local discomfort in 22 (15.7%); local pain at rest, on movement or associated with exercise in 16 (11.5%) to 5 (3.6%); an inguinal bulge in 5.8%; associated GP visit(s) in 5.0%; change in testis size in 3.0%; analgesic use for inguinal pain in 2.9%; associated sick leave in 2.1%; and, no hernia recurrences. When all pain-related questions (A to G) were combined, 17.0% (24/141) of participants had some degree of chronic pain.
Table 2 shows that the frequency distribution of adverse responses was skew where the majority 72 (51.1%) participants recorded no adverse responses and nine (6.4%) reported five or more. Table 2 also shows that those participants who registered few adverse responses more frequently complained of sensation of material under the skin, abnormal local skin sensation and discomfort. Those participants who registered many abnormal responses more frequently complained of chronic pain issues.
 Click to view | Table 2. Frequency of Numbers and Types of Adverse Responses |
Significant associations were observed between a positive response to any pain question (A to G) and: the sensation of repair material (P = 0.001); local discomfort (P = 0.002); and, abnormal skin sensation (P = 0.005). The length of participant follow-up time was not associated with the presence of any MIS symptoms (all P ≥ 0.263).
| Discussion | ▴Top |
Postal surveys using patient-completed questionnaires have been previously used to assess the long-term outcomes of open inguinal herniorrhaphy [6, 8, 9]. Their accuracy and utility are largely determined by the quality of the design and validation processes used for the questionnaires [10, 11].
The questionnaire used for our survey was previously employed by others who also included additional data from selected patient telephone interviews and clinical evaluations. This study had response rates of 78.3% at 2 years and 77.6% at 5 years of follow-up [6]. Our survey had a lower response rate of 67.8% after a mean of 3.11 years. This lower rate may have been because we did not contact participants to collect additional clinical data. Perhaps the major reason may have been the considerable population disruption after the Canterbury earthquakes of 2010 and 2011. Our sample size should be large enough, however, to permit some valid conclusions about clinical outcomes.
Our survey showed a very low incidence of participant-reported acute post-operative complications, including some self-limiting wound problems, but no serious adverse events. This compares favourably with those reported elsewhere [12-14].
Long-term outcomes
Regarding impact on general lifestyle, during the previous year 5% of participants visited a GP with problems due to the inguinal hernia surgery and 2.1% needed some related sick leave. Evaluation of responses to questions on groin bulges and changes in testis size would require individual participant evaluations. They are therefore not discussed.
No inguinal hernia recurrences and no surgery for hernia recurrences were reported in our survey. These results are typical of the findings with tension-free hernia operations of the Lichtenstein-type [15, 16]. Since their introduction, MIS has been increasingly recognized as the main long-term problem. This constellation of chronic local neuropathic and nociceptive symptoms is thought to be due to local nerve injury and chronic inflammation associated with the surgery and the repair materials [4].
Previous studies addressing the frequencies of MIS symptoms are beset with inconsistencies of definitions, data collection and reporting [17]. These inconsistencies are typified by the varying ranges of reported chronic pain of 4% to 62% [18, 19]. In our survey, when all questionnaire responses were combined for pain (at rest, on movement; affecting everyday life; preventing sport or exercise; and, requiring analgesia), 17.0% of participants had some degree of chronic pain. A recent study has shown that, in spite of an appreciable incidence of post-open inguinal herniorrhaphy pain, the majority of patients reported significant improvement in quality of life measures, pain scores and symptoms, even those with mild symptoms before surgery [20]. The reported incidences of MIS symptoms in our survey, however, prompted desire for improvement.
Other MIS symptoms recorded in our survey included a sensation of repair material under the skin in 18.6%, abnormal local skin sensation in 30.7%, and local discomfort in 15.7%. These frequencies were similar to those recorded in previous studies [6, 19]. All three symptoms correlated positively with some of the chronic pain questions. Our data are therefore consistent with the notion of a common etiology for these MIS symptoms.
The absence of a significant positive correlation between MIS symptoms and length of participant follow-up in our data does not correspond with the commonly espoused opinion that symptoms improve with time. It is, however, in line with the results of previous studies [6, 9].
Risk factors for MIS
A large number of pre-, peri- and post-operative risk factors have been identified for MIS [4]. These include young age, female gender, high levels of pre-operative pain and some psychological factors. Numerous randomized controlled trials (RCTs) have investigated some of these factors in order to reduce the incidence and/or severity of MIS symptoms [17]. For CCH, it would likely be the most advantageous to address the type of repair material.
Alternative repair materials
Many new materials with different physical and biological properties have been produced for hernia repairs [21]. RCTs and meta-analyses of studies comparing some of these different materials have produced varied and indefinite conclusions on the optimum types and methods to use [22-26]. For example, a single surgeon RCT compared a partially absorbable mesh with lightweight and heavyweight Prolene meshes. After 5 years of follow-up, there were no differences in hernia recurrence rates, feeling of foreign material under the skin, pain or analgesic usage [27].
A recent meta-analysis of 16 RCTs and five comparative studies, however, showed that lightweight meshes were associated with less MIS symptoms than heavyweight meshes but raised concerns that they might have higher recurrence rates when used to repair large hernias [28]. Another similar meta-analysis of nine RCTs also showed that lightweight meshes were associated with lower incidences of MIS symptoms but demonstrated no increased risk of hernia recurrence [29].
As a result of our survey, CCH now uses a lightweight Prolene mesh. The survey will be repeated in future to assess whether this change has reduced the frequency of MIS symptoms without affecting the hernia recurrence rate. Patient-reported surveys, such as the one used in our survey, are potentially useful tools for the assessment of long-term surgical outcomes. They might be particularly so in situations where there are technical controversies.
Acknowledgement
The authors wish to thank Mr Georgios Pierides, Ambulatory Surgery Unit of Jorvi Hospital, Helsinki University Central Hospital, Finland who provided the questionnaire for this survey; Professor Risto Kaaja, Turku Central Hospital and Turku University, Turku, Finland who translated it into English; volunteers and staff of CCH for assistance with data collection; and Ms Jenah Shaw for editorial assistance.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
Canterbury Charity Hospital Trust.
| References | ▴Top |
- Bagshaw PF, Maimbo-M'siska M, Nicholls MG, Shaw CG, Allardyce RA, Bagshaw SN, McNabb AL, et al. The Canterbury Charity Hospital: an update (2010-2012) and effects of the earthquakes. N Z Med J. 2013;126(1386):31-42.
pubmed - Kockerling F, Schug-Pass C. Tailored approach in inguinal hernia repair - decision tree based on the guidelines. Front Surg. 2014;1:20.
pubmed - Basile F, Biondi A, Donati M. Surgical approach to abdominal wall defects: history and new trends. Int J Surg. 2013;11(Suppl 1):S20-23.
doi - Bjurstrom MF, Nicol AL, Amid PK, Chen DC. Pain control following inguinal herniorrhaphy: current perspectives. J Pain Res. 2014;7:277-290.
pubmed - Heise CP, Starling JR. Mesh inguinodynia: a new clinical syndrome after inguinal herniorrhaphy? J Am Coll Surg. 1998;187(5):514-518.
doi - Pierides G, Vironen J. A prospective randomized clinical trial comparing the Prolene Hernia System(R) and the Lichtenstein patch technique for inguinal hernia repair in long term: 2- and 5-Year results. Am J Surg. 2011;202(2):188-193.
doi pubmed - Lichtenstein IL, Shulman AG. Ambulatory outpatient hernia surgery. Including a new concept, introducing tension-free repair. Int Surg. 1986;71(1):1-4.
pubmed - Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U. Risk factors for long-term pain after hernia surgery. Ann Surg. 2006;244(2):212-219.
doi pubmed - Bay-Nielsen M, Perkins FM, Kehlet H. Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg. 2001;233(1):1-7.
doi pubmed - Statistics Canada: Questionnaire design. [Cited 20 Feb 2015.] Available from URL: http://www.statcan.gc.ca/pub/12-539-x/2009001/design-conception-eng.htm
- Franneby U, Gunnarsson U, Andersson M, Heuman R, Nordin P, Nyren O, Sandblom G. Validation of an Inguinal Pain Questionnaire for assessment of chronic pain after groin hernia repair. Br J Surg. 2008;95(4):488-493.
doi pubmed - Magnusson J, Nygren J, Thorell A. Lichtenstein, prolene hernia system, and UltraPro Hernia System for primary inguinal hernia repair: one-year outcome of a prospective randomized controlled trial. Hernia. 2012;16(3):277-285.
doi pubmed - Vironen J, Nieminen J, Eklund A, Paavolainen P. Randomized clinical trial of Lichtenstein patch or Prolene Hernia System for inguinal hernia repair. Br J Surg. 2006;93(1):33-39.
doi pubmed - Kingsnorth AN, Wright D, Porter CS, Robertson G. Prolene Hernia System compared with Lichtenstein patch: a randomised double blind study of short-term and medium-term outcomes in primary inguinal hernia repair. Hernia. 2002;6(3):113-119.
doi pubmed - Gupta A, Jain SK, Kumar S, Kaza RCM. Laparoscopic vs. open inguinal hernia repair: a systemic review of literature. Asian J Med Sci. 2014;5(3):10-14.
doi - O'Reilly EA, Burke JP, O'Connell PR. A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg. 2012;255(5):846-853.
doi pubmed - Bhangu A, Singh P, Pinkney T, Blazeby JM. A detailed analysis of outcome reporting from randomised controlled trials and meta-analyses of inguinal hernia repair. Hernia. 2015;19(1):65-75.
doi pubmed - Jeroukhimov I, Wiser I, Karasic E, Nesterenko V, Poluksht N, Lavy R, Halevy A. Reduced postoperative chronic pain after tension-free inguinal hernia repair using absorbable sutures: a single-blind randomized clinical trial. J Am Coll Surg. 2014;218(1):102-107.
doi pubmed - Pierides G, Scheinin T, Remes V, Hermunen K, Vironen J. Randomized comparison of self-fixating and sutured mesh in open inguinal hernia repair. Br J Surg. 2012;99(5):630-636.
doi pubmed - Palmqvist E, Larsson K, Anell A, Hjalmarsson C. Prospective study of pain, quality of life and the economic impact of open inguinal hernia repair. Br J Surg. 2013;100(11):1483-1488.
doi pubmed - Bilsel Y, Abci I. The search for ideal hernia repair; mesh materials and types. Int J Surg. 2012;10(6):317-321.
doi pubmed - Kockerling F, Schug-Pass C. What do we know about titanized polypropylene meshes? An evidence-based review of the literature. Hernia. 2014;18(4):445-457.
doi pubmed - Zhong C, Wu B, Yang Z, Deng X, Kang J, Guo B, Fan Y. A meta-analysis comparing lightweight meshes with heavyweight meshes in Lichtenstein inguinal hernia repair. Surg Innov. 2013;20(1):24-31.
doi pubmed - Smietanski M, Smietanska IA, Modrzejewski A, Simons MP, Aufenacker TJ. Systematic review and meta-analysis on heavy and lightweight polypropylene mesh in Lichtenstein inguinal hernioplasty. Hernia. 2012;16(5):519-528.
doi pubmed - Sanjay P, Watt DG, Ogston SA, Alijani A, Windsor JA. Meta-analysis of Prolene Hernia System mesh versus Lichtenstein mesh in open inguinal hernia repair. Surgeon. 2012;10(5):283-289.
doi pubmed - Zhao G, Gao P, Ma B, Tian J, Yang K. Open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Ann Surg. 2009;250(1):35-42.
doi pubmed - Paajanen H, Ronka K, Laurema A. A single-surgeon randomized trial comparing three meshes in lichtenstein hernia repair: 2- and 5-year outcome of recurrences and chronic pain. Int J Surg. 2013;11(1):81-84.
doi pubmed - Li J, Ji Z, Cheng T. Lightweight versus heavyweight in inguinal hernia repair: a meta-analysis. Hernia. 2012;16(5):529-539.
doi pubmed - Sajid MS, Leaver C, Baig MK, Sains P. Systematic review and meta-analysis of the use of lightweight versus heavyweight mesh in open inguinal hernia repair. Br J Surg. 2012;99(1):29-37.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.