| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Original Article
Volume 6, Number 3-4, December 2016, pages 65-72
A Comparative Study of Polydioxanone and Nylon for Abdominal Wall Closure With Interrupted Figure of Eight in Peritonitis Cases
Rikki Singala, c, Mohinder Kumara, Nitin Kaushikb, Siddharth Dhara, Bir Singha
aDepartment of Surgery, Maharishi Markandeshwer Institute of Medical Sciences and Research, Mullana, (Distt-Ambala), Haryana, India
bDepartment of Surgery, Maharishi Markandeshwer Institute of Medical Sciences and Research, Solan, Himachal, India
cCorresponding Author: Rikki Singal, C/o Dr Kundan Lal Hospital, Ahmedgarh, Distt-Sangrur, Punjab 148021, India
Manuscript accepted for publication September 15, 2016
Short title: Abdominal Wall Closure in Peritonitis Cases
doi: https://doi.org/10.14740/jcs306e
| Abstract | ▴Top |
Background: In emergency and elective settings, some surgeons prefer continuous or interrupted closure of abdominal fascia, because in a continuous suturing, cutting out of even a single bite of tissue leads to opening of the entire wound and high risk of burst abdomen, whereas in interrupted method, they found much lower risk of burst abdomen. The aim is to assess the complication rate with the same closure technique between two different sutures. The best suture is one that maintains tensile strength throughout the healing process with good tissue approximation and less wound infection, is well tolerated by patient and is technically simple and expedient. The aim was to compare the non-absorbable sutures (nylon) and delayed absorbable sutures (polydioxanone (PDS)) for abdominal wall closure in cases of peritonitis. We used a different technique to close the abdominal wall fascia and study the postoperative complications.
Methods: This was a prospective study carried out in the Department of Surgery, MMIMSR, Mullana, Ambala from March 2014 to April 2015, a single unit by a single surgeon. A total of 60 patients underwent interrupted closure of abdominal fascia by figure of eight techniques with polyamide (nylon No. 1) suture in group A and polydiaxanone (PDS No. 1) suture in group B. The incidence rates of wound infection, dehiscence, suture sinus formation and incisional hernia were recorded. Patients were followed up for a period of 1 year.
Results: Out of the 60 patients, the rates of wound pain, discharge and dehiscence in group A were 30%, 23.3% and 26.7% and in group B were 6.7%, 16.6% and 23.3%. There was 0 burst abdomen in group A compared to one burst abdomen in group B. Suture sinus formation, chronic wound infection and stitch granuloma was one each in group A and was 0 in group B. Incisional hernia was not found in any of the group. We have concluded that condition of the wound depends on the comorbidity of the patient like smoking, malnutrition, and old peritonitis. It also mainly depends on the technique used for closure of the wound and also on the material used.
Conclusion: Though wound complications were found more in non-absorbable suture but the rate of wound complications between the two sutures was found insignificant. The purpose of the study is to assess the presence of differences in abdominal wall closure in patients with risk criteria, with the same closure technique between slowly absorbable sutures and non-absorbable sutures. Sutures were placed and tied such that fascial edges were well approximated but not compressed tightly together.
Keywords: Peritonitis; Abdominal wall closure; Abdominal wound; Suture material; Complications
| Introduction | ▴Top |
Every surgeon’s dream is to close the abdominal incisions securely, so as to prevent complications, such as wound infections, dehiscence, incisional hernia and sinuses. The closure of the dehisced abdominal wound after a major wound infection is a challenging problem as it is usually accompanied with a tissue loss [1]. The purpose of the suture material is to hold the abdominal wall layer together in good apposition until such time as the natural healing process is sufficiently well established.
Polydioxanone (PDS) provides prolonged wound support by retaining its tissue integrity longer than other synthetics absorbable. The PDS sutures loose half of their mechanical strength in about 3 weeks and complete degradation takes place in around 6 months. Laparotomy closure with an absorbable material should decrease the incidence of postoperative wound pain and persistent suture sinuses. On the other hand, non-absorbable materials retain their strength in the process of healing to minimize the occurrence of incisional hernia. Absorbable materials are designed to approximate the sheath during the critical early healing period and subsequently to undergo absorption to avoid the complications of sinus formation, pain, and buttonhole hernia associated with non-absorbable sutures. In emergency and elective settings, some surgeons prefer to do continuous closure of abdominal fascia, while others prefer interrupted suture because they found that in a continuous suturing, cutting out of even a single bite of tissue leads to opening of the entire wound and high risk of burst abdomen, whereas in interrupted method of closure, they found much lower risk of burst abdomen. The ideal suture for abdominal fascia has yet to be determined. In this study, we hope to shed some light on this debatable topic, using interrupted technique in all cases.
| Materials and Methods | ▴Top |
All peritonitis cases of either sex, presenting to the Department of the General Surgery, MMIMSR, Mullana, MM University, Ambala at tertiary care teaching hospital, India, from March 2014 to April 2015 were assessed in the prospective study. The study was approved by the institutional ethics committee. The study included 60 patients with peritonitis who were divided into two groups (A and B) randomly. In each group A and group B, 30 patients (totally 60 patients) underwent interrupted closure of abdominal fascia with polyamide (nylon) No. 1 suture in group A and polydioxanone (PDS) No.1 suture in group B with technique of eight. Wherever possible, comorbid factors were corrected such as anemia, hypertension, and diabetes mellitus. Patients admitted in emergency diagnosed as peritonitis and age more than 10 years were included in the study. Patients with pre- or postoperative diagnosis of malignant involvement of peritoneum, severe renal and liver disease, uncontrolled diabetes or on chemotherapy/steroids were excluded from the study.
All the required investigations were done to make the diagnosis: complete hemogram, urine examination, serum electrolytes, blood sugar, blood urea and serum creatinine, X-ray abdomen (erect), chest X-ray, USG abdomen, ECG and other relevant investigations accordingly. After taking detailed history and examination for the underlying cause of peritonitis, all patients were given preoperative dose of antibiotics (ceftriaxone, gentamycin and metronidazole) which was also continued in the postoperative period according to renal status.
Surgical technique
Exploratory laparotomy was carried out through a midline vertical incision through the subcutaneous layer. After correction of primary cause, thorough peritoneal lavage was given. The required abdominal fascial closure was done accordingly. In group A, non-absorbable monofilament No. 1 polyamide (nylon) was used in an interrupted figure of eight manner taking four squared knots in a single suture tie (Fig. 1). The bites were taken 1.5 cm away from the cut margin and at a distance of 1 cm between each other (Fig. 2). Each knot was buried to avoid sinus formation and it would not cause irritation to patient postoperatively. In group B, delayed absorbable monofilament No. 1 PDS was used in a similar interrupted manner taking 6 - 8 squared knots in a single suture tie.
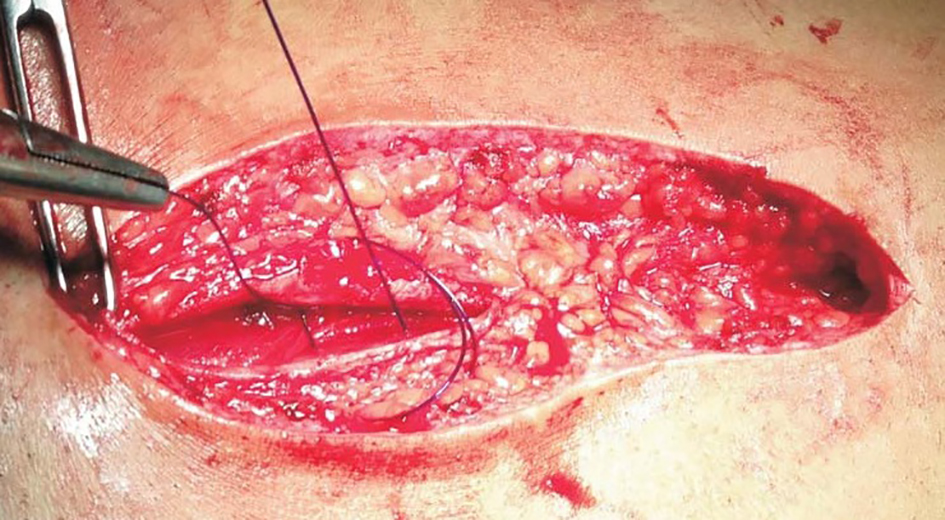 Click for large image | Figure 1. Bite is taken 1.5 cm from cut edge of linea alba on the opposite side. |
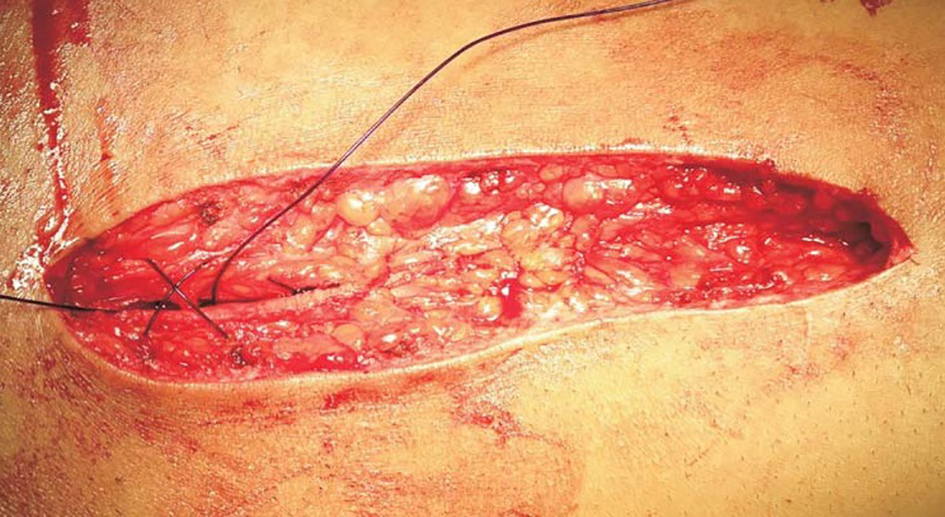 Click for large image | Figure 2. Ends are tied which creates figure of eight. |
No subcutaneous or drainage is inserted. The skin is closed with skin clips or interrupted sutures with monofilament non-absorbable sutures. The primary dressing was removed after 24 h and daily dressing was done with providence-iodine solution. The wound was inspected for signs of infection and dehiscence before each dressing. Patients were then being put on antibiotics according to the culture and sensitivity report if they showed any systemic sign of infection.
At the end of the study, the two groups were compared in early and late complications. Early complications were wound pain, discharge, dehiscence and burst abdomen. Late complications were chronic wound infection, suture sinus formation, incisional hernia, stitch granuloma. Other details which were recorded included duration of hospital stay, drain used or not, approximate length of incision, antibiotics used, and complications if any. Follow-up was conducted at 7, 30, and 90 days to assess the wound. The data thus obtained were tabulated using Microsoft Excel.
Observations and analysis
The study included 60 patients undergoing closure of abdominal fascia by No. 1 suture polyamide (nylon) in group A and PDS in group B with interrupted technique as eight- shaped. Sixteen patients (53.3%) were in the second and third decades of life in group A, whereas 12 patients (40 %) were in the second and third decade of life in group B. Majority of the patients (28/60) were in the second and third decade of life. So peritonitis is a disease of young adults and middle aged. Only 11 of 60 patients (13.3%) were beyond the seventh decade of life in each group. The mean age in our study was 36.7 years, median was 35.0 and standard deviation was 18.2. The majority of patients in group A (21 patients or 70 %) and in group B (20 patients or 66.7 %) were male. Male to female ratio in our study was 2.16:1. The heavy preponderance of males could be due to more use of intoxication like alcohol, smoking, irregular meals, more outdoor life and eating spicy foods. All of them contributed to small bowel pathologies.
The most common presenting complaint was abdominal pain. Most of the patients presented with pain abdomen, abdominal distention, vomiting and altered bowel habit. Twenty-six (43.3%) patients had history of fever. In group A, 13 patients were smoker and in group B, 10 patients were smoker; whereas three patients were alcoholic in group A and eight patients were alcoholic in group B. One tobacco chewer was found in each group and drug addiction was 0 in group A and one in group B. A total of 35 (58.3%) patients had associated comorbidities.
The most common site of perforation was duodenal in group A and was ileal in group B, followed by pre-pyloric and ileal in group A and duodenal, gastric and pyloric in group B (Fig. 3). Least common site was Meckel’s diverticulum and sigmoid. Duodenal, pyloric, pre-pyloric and gastric perforations were mainly due to sequel of peptic ulcer. Patients had peritonitis without perforation. They had pus collection in abdominal cavity and totally two patients had jejunal perforation, which was due to trauma. Appendiceal perforation was sequel of acute appendicitis. Sigmoid perforation was sequel of colorectal carcinoma whereas Meckel’s diverticulum was due to Meckel’s diverticulitis. In both groups, ileal perforation was more common in 11 - 30 years of age group, meaning typhoid ulcers more commonly occurred in young adult age. Duodenal and pre-pyloric perforations were more commonly found in 21 - 40 years of age group, which means peptic ulcers were more commonly found in adult and middle age group (Table 1).
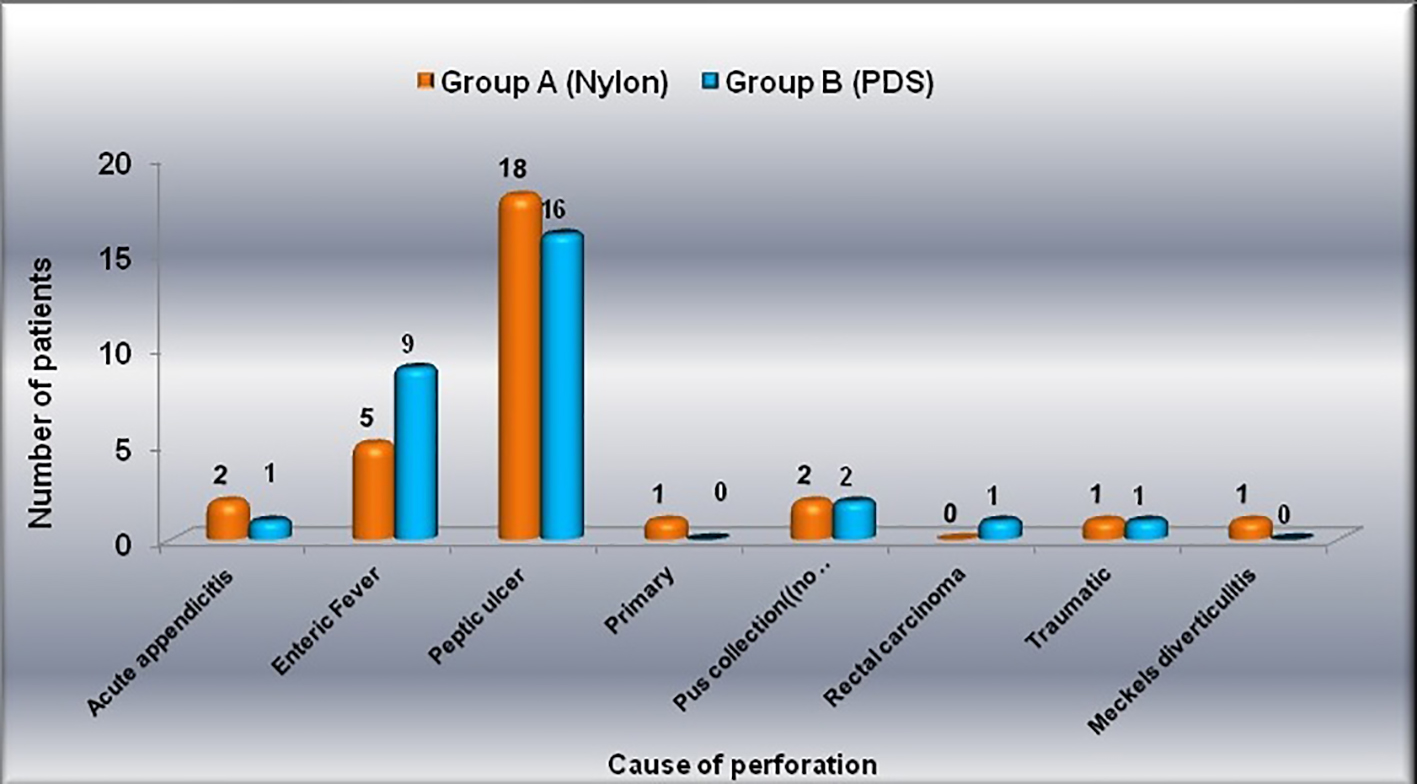 Click for large image | Figure 3. Distribution of patients according to cause of perforation in both groups (separately). |
 Click to view | Table 1. Age Distribution of Patients According to Site of Perforation |
The wound pain was evaluated; in nylon group, it was found to be 30% as compared to 6.7% in PDS group (Table 2 and Table 3 [2-4]). However, this difference was found to be statistically insignificant. Wound pain occurred more frequently with nylon suture because of its long memory, more tissue reaction and stiff nature. Wound pain occurred less frequently with the use of PDS because it had been found to be non-antigenic, non-pyrogenic and elicited only minimal tissue reactivity during the absorption process. The wound discharge rate was found to be 23.3% in nylon group as compared to 16.7% in PDS group. However, this difference was found to be statistically insignificant. This was because both the sutures were monofilament used in our study preventing wound discharge (Table 4) [4-7]. The wound dehiscence occurred (26.7%) in group A and (23.3%) in group B. Delayed absorbable suture was comparable to non-absorbable suture in terms of wound dehiscence which was found to be better because PDS sutures loosed half of their mechanical strength in about 3 weeks, thus providing wound support for longer periods. So delayed absorbable sutures were equally effective in infected cases like peritonitis (Fig. 4).
 Click to view | Table 2. Outcomes of Wound |
 Click to view | Table 3. Wound Pain |
 Click to view | Table 4. Wound Discharge |
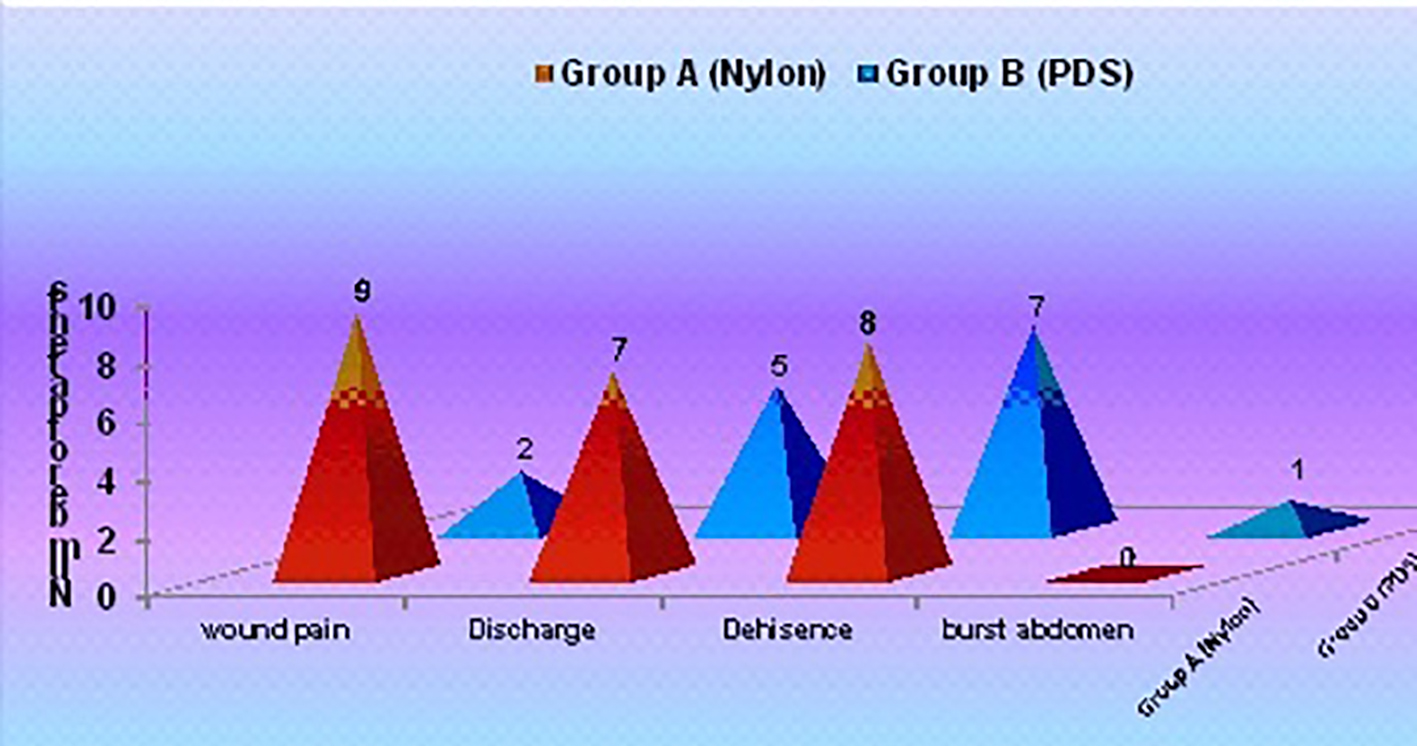 Click for large image | Figure 4. Early wound complications in the two groups. |
Burst abdomen rate was found to be 0% in nylon group as compared to 3.3% in PDS group. However, this difference was found to be statistically insignificant. This is because both the sutures were monofilament used in our study (Table 2). The rate of prevalence of chronic wound infection in group A was 3.3% in comparison to group B which was 0%. This difference was found to be statistically insignificant (Fig. 5). The suture sinus rate was found to be 3.3% in nylon group as compared to 0% in PDS group. However, this difference was found to be statistically insignificant. Suture sinus occurred more frequently with nylon suture because of its long memory and stiff nature. Sinus formation occurred less frequently with the use of PDS because it had been found to be smooth, pliable and minimal memory (Table 5) [4, 8, 9].
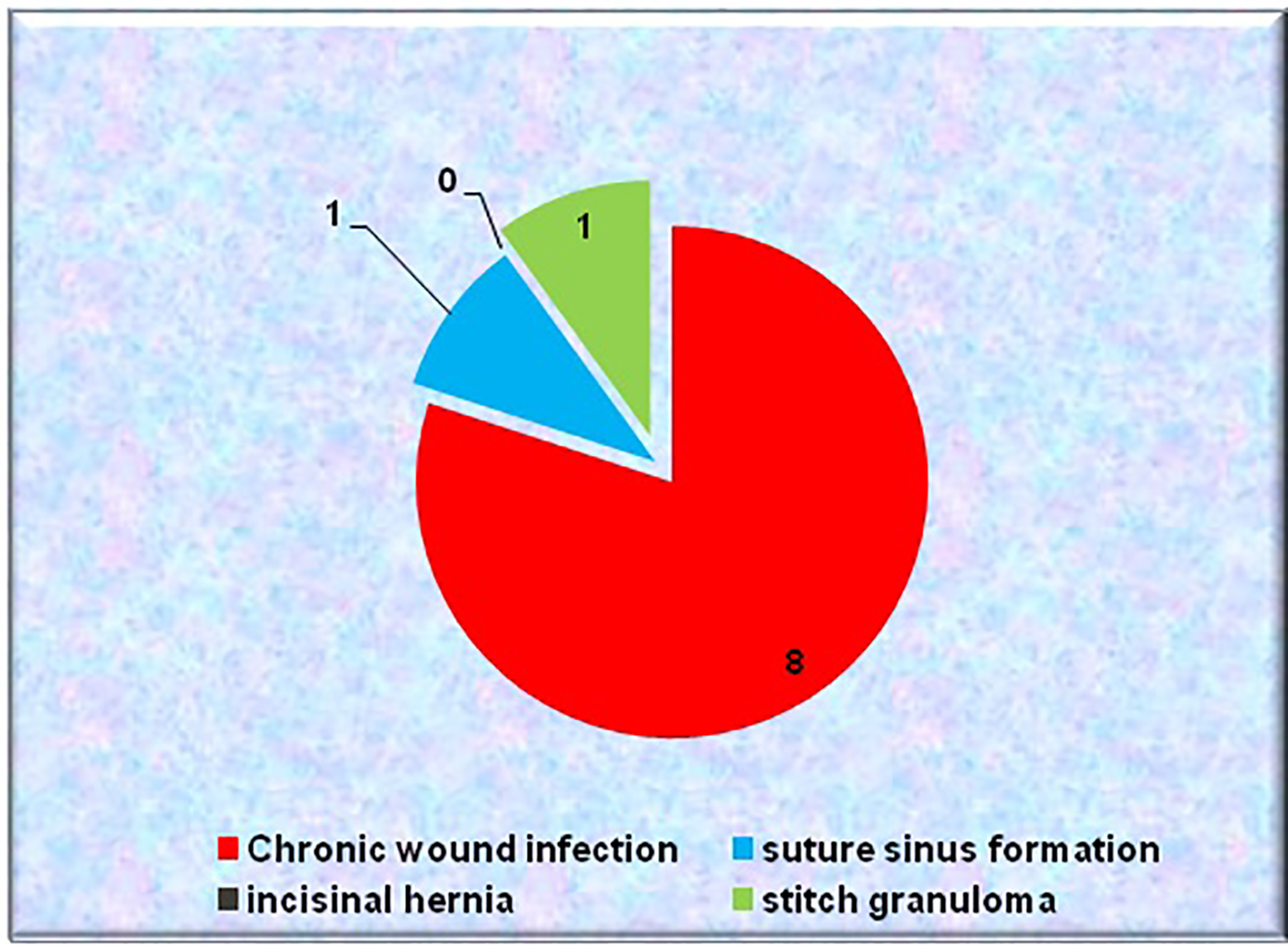 Click for large image | Figure 5. Distribution of late wound complications among patients. |
 Click to view | Table 5. Suture Sinus Formation |
The incisional hernia did not occur in any of the group in our study. This was probably due to interrupted technique of fascia closure, in which if any of suture was cut through, rest of sutures retained the fascia in opposition. Delayed absorbable and non-absorbable sutures were comparable in terms of incisional hernia incidence because PDS sutures loosed half of their mechanical strength in about 3 weeks and complete degradation took place in around 6 months, thus providing wound support for longer periods and reducing the chances of hernia formation (Table 6) [4, 6, 9-11]. In nylon group, stitch granuloma rate was found to be 3.3% as compared to 0% in PDS group. However, this difference was found to be statistically insignificant. Stitch granuloma occurred with nylon suture because of its long memory and stiff nature.
 Click to view | Table 6. Incisional Hernia |
| Discussion | ▴Top |
The best method of wound closure would be to provide adequate tensile strength until the wound is healed, approximate the tissue in a way that normal healing mechanisms can occur under optimal circumstances, and remain secure even in the presence of local or systemic infection. Sajid et al studied that PDS was comparable to prolene/nylon in terms of risk of incisional hernia, wound dehiscence, peri-operative complications, suture sinus formation and surgical site infection, given that there are no significant differences between two suture materials [8]. Another study declared that closure by continuous rapidly absorbable suture results in more incisional hernias than closure by continuous slowly absorbable suture. But wound pain and suture sinuses occurred more after the use of non-absorbable suture [2]. A study stated that a non-absorbable or slowly absorbed suture such as PDS is the method of choice for abdominal wall closure. PDS has a similar incisional hernia rate to its non-absorbable counterparts but causes less chronic pain and wound sinuses [12]. Hohlagschwandtner et al stated that continuous single-layer closure of rectus sheath saves operating time, reduces blood loss, and introduces less foreign material into the wound [13]. Srivastava et al resulted that in X suture group, only one had burst abdomen and in the continuous group eight had burst abdomen. The risk of burst abdomen in the emergency group is less with interrupted X method of closure as seen in our study [14].
Bellon et al evaluated the long-lasting absorbable material PDS 4/0 and a non-absorbable material polypropylene 4/0 with an en masse running suture in 48 New Zealand White rabbits. No significant differences were found in the biomechanical strength provided by the two types of suture. The composition of the suture material did not affect the tensile strength of the repair zone [15]. Eshghi et al concluded that no significant difference in the rate of hernia, infection and wound dehiscence was found in two types of suture PDS/nylon. However, application of PDS led to less postoperative pain and sinus formation [16]. Our results were also matching to the above study.
Docobo-Durantez et al stated the surgical infection rate was 10%, and wound pain was more with nylon as compared to PDS. They concluded that abdominal wall closure should be performed with slow-absorption sutures such as PDS since this type of suture has a similar complication rate to non-absorbable sutures [3]. Gaikwad et al declared an alarmingly higher incidence of wound dehiscence in the PDS group than nylon group. There was, however, a statistically significantly higher incidence of scar pain in the nylon group (nylon 9; PDS 1) [17]. In the current study, wound pain occurred more frequently in nylon group though not significant. Wound pain occurred more frequently with nylon suture because of its long memory, more tissue reaction and stiff nature. Wound pain occurred less frequently with the use of PDS because it had been found to be smooth, pliable, minimal memory, non-antigenic, non-pyrogenic and elicited only minimal tissue reactivity during the absorption process.
Khan et al showed the postoperative wound discharge rate of 24% in the non-absorbable group (polyamide) and 16% in the absorbable group (polyglyconate). They concluded that slowly absorbable suture material appears to be superior to non-absorbable suture material in midline abdominal fascial closure [4]. Bloemen et al conducted a study on 456 patients to close the abdominal fascia with either non-absorbable (prolene) or absorbable (PDS) suture material. There was no significant difference in the incidence of incisional hernia between the groups: 20.2% (45 of 223) for prolene and 24.9% (58 of 233) for PDS (P = 0.229) [10].
Yadav and Garg reported that majority of the patients (96.6%) presented with the history of pain in abdomen, 73.9% with abdominal distention, 55.7% with altered bowel habit and 52.3% with nausea vomiting [9]. Jhobta et al found that pain abdomen was present in 495 (98%), vomiting in 296 (59%), abdominal distention in 221 (44%), constipation in 193 (38%), fever in 124 (25%), and diarrhea in 35 (7%) patients in perforation peritonitis cases [18]. Seiler et al conducted a study using continuous or interrupted technique with various suture materials and found that wound discharge was 12.7% vs. 19.4% vs. 16.3% in three different groups (P = 0.19) [5]. Altaf et al conducted a randomized study on 274 patients for wound discharge rate which was found to be 6.61% (non-absorbable group) and 5.7% (absorbable group) [6]. Hisham et al studied 126 patients who were divided into two groups of absorbable and non-absorbable suture material. The wound discharge rate was 25% and 28.7%, respectively in above groups [7].
The wound discharge was not found to be statistically affected by the suture material employed because both the sutures were monofilament used in present study and both had minimal tissue reaction. No statistically significant difference in wound discharge rates was observed with either suture. In the current study, wound dehiscence occurred in eight patients in group A and in seven patients in group B. Khan et al conducted a prospective, randomized study and found that there was a total of three wound dehiscence in both the groups [4]. So it is clear from above studies that delayed absorbable suture comparable to non-absorbable suture in terms of wound dehiscence is little better, because PDS sutures loose half of their mechanical strength in about 3 weeks, thus providing wound support for longer periods.
Sajid et al conducted a study and reported that there was a higher incidence of suture sinus formation when non-absorbable suture material was used [8]. Present study showed that non-absorbable sutures are associated with more sinus formation than delayed absorbable sutures because of their long memory and stiff nature. Sinus formation occurred less frequently with the use of delayed absorbable (PDS) because it has been found to be smooth, pliable and minimal memory. Altaf et al conducted a randomized study with non-absorbable (nylon) and absorbable (PDS) sutures and found that the rate of incisional hernia which was 4.34% more with nylon than 0.73% with (PDS) [6]. Above studies had no significant difference in incidence of incisional hernia rate between non-absorbable and delayed absorbable sutures. Present study also showed same results but we had 0% hernia rate in both the groups, which was probably due to interrupted technique of fascia closure, in which if any of suture was cut through, rest of sutures retained the fascia in opposition. Israelsson and Jonsson (1994) conducted a randomized clinical trial in which they evaluated the healing of midline laparotomy incisions closed with a continuous suture of nylon or second-generation polydioxanone. Wound dehiscence occurred in five (0.6%) of 813 patients and wound infection in 73 (9.0%). These rates were similar for both suture materials. These results indicate that suture of midline laparotomy wounds is as safe with polydioxanone as it is with nylon. Incisional hernia is associated more with suture technique than with the material used [11].
The mean duration of hospital stay while using nylon was 17.0 ± 8.7 days as compared to 20.1 ± 11.4 days for PDS suturing. The duration of hospital stay was nearly similar in both the suture material because none of them have significantly more wound complications. According to our study, we were able to conclude that, though wound complications with non-absorbable sutures were found to be more compared to delayed absorbable suture, but the rates of wound complications between the two sutures were found insignificant and also with use of interrupted suturing with figure of eight technique, the strength of wound became more and there are much less chances of incisional hernia and burst abdomen. One more advantage of nylon is that it is cheaper as compared to PDS. Despite advancements in surgical techniques, antimicrobial therapy and intensive care, management of peritonitis continues to be highly challenging. Factors contributing to the high mortality and postoperative complications are advanced age, late presentation, delay in the treatment, septicemia, and associated comorbidity [19].
Distinctive characteristics of PDS sutures are: 1) PDS is non-antigenic, non-pyrogenic and elicits only minimal tissue reactivity during the absorption process; 2) smooth, pliable and minimal memory; 3) other trials have stated that PDS handles knots as well as catgut. Nylon sutures have the following distinctive characteristics: 1) non-absorbable and good tensile strength; 2) good elasticity; 3) easy passage through tissues due to low friction coefficient; 4) eliciting minimal inflammatory reaction in tissues; 5) even though it is non-absorbable, the knot security decreases over time and is not preferred where permanent retention is required.
Conclusion
The ideal method of wound closure would be one that provides adequate tensile strength to the tissues until the wound has healed. One of our analyses made in burst abdomen showed advantage of non-absorbable suture over delayed absorbable suture. But we want to also add that burst abdomen or other complications depend upon the technique used for closure, and on systemic factors. In our study, though wound pain, discharge, dehiscence and suture sinus formation were found in non-absorbable sutures, there was not much difference as compared to absorbable sutures.
Conflicts of Interest
None.
Funding Source
None.
| References | ▴Top |
- Abbasoglu O, Nursal T. Surgical technique for closure of difficult abdomen. Acta Chir Belg. 2003;103(3):340-341.
doi pubmed - van 't Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J. Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg. 2002;89(11):1350-1356.
doi pubmed - Docobo-Durantez F, Sacristan-Perez C, Flor-Civera B, Lledo-Matoses S, Kreisler E, Biondo S. [Randomized clinical study of polydioxanone and nylon sutures for laparotomy clousure in high-risk patients]. Cir Esp. 2006;79(5):305-309.
doi - Khan NA, Danish A, Khubaib S, Khan A, Mian MA, Murt B. Comparison between delayed-absorbable polydioxanone and non-absorbable (prolene) suture material in abdominal wound closure. Pafm J Surg. 2009;2.
- Seiler CM, Bruckner T, Diener MK, Papyan A, Golcher H, Seidlmayer C, Franck A, et al. Interrupted or continuous slowly absorbable sutures for closure of primary elective midline abdominal incisions: a multicenter randomized trial (INSECT: ISRCTN24023541). Ann Surg. 2009;249(4):576-582.
doi pubmed - Altaf A, Fatmi Z, Ajmal A, Hussain T, Qahir H, Agboatwalla M. Determinants of therapeutic injection overuse among communities in Sindh, Pakistan. J Ayub Med Coll Abbottabad. 2004;16(3):35-38.
pubmed - Hisham El-Sharkawy, Hatem H, Engie H. Midline abdominal Wound Closure A Randomized Prospective Study of 105 Patients Comparing Continuous vs. Interrupted Suture Techniques. Kasr El Aini J Surg. 2007;8:47-54.
- Sajid MS, Parampalli U, Baig MK, McFall MR. A systematic review on the effectiveness of slowly-absorbable versus non-absorbable sutures for abdominal fascial closure following laparotomy. Int J Surg. 2011;9(8):615-625.
doi pubmed - Yadav D, Garg PK. Spectrum of perforation peritonitis in delhi: 77 cases experience. Indian J Surg. 2013;75(2):133-137.
doi pubmed - Bloemen A, van Dooren P, Huizinga BF, Hoofwijk AG. Randomized clinical trial comparing polypropylene or polydioxanone for midline abdominal wall closure. Br J Surg. 2011;98(5):633-639.
doi pubmed - Israelsson LA, Jonsson T. Closure of midline laparotomy incisions with polydioxanone and nylon: the importance of suture technique. Br J Surg. 1994;81(11):1606-1608
- O'Dwyer PJ, Courtney CA. Factors involved in abdominal wall closure and subsequent incisional hernia. Surgeon. 2003;1(1):17-22.
doi - Hohlagschwandtner M, Chalubinski K, Nather A, Husslein P, Joura EA. Continuous vs interrupted sutures for single-layer closure of uterine incision at cesarean section. Arch Gynecol Obstet. 2003;268(1):26-28.
pubmed - Srivastava A, Roy S, Sahay KB, Seenu V, Kumar A, Chumber S, et al. A randomized trial comparing continuous versus interrupted X-suture. Indian J Surg. 2004;66:19-27.
- Bellon JM, Rodriguez M, Serrano N, Garcia-Honduvilla N, Gomez V, Bujan J. [Polypropylene and polydioxanone show similar biomechanical efficacy in midline closure]. Cir Esp. 2005;78(6):377-381.
doi - Eshghi F, Khalilian AR, Jamshidi M. Comparison of PDS and nylon sutures complications in abdominal midline repair. Journal of Mazandaran University of Medical Sciences. 2006;16:1-6.
- Gaikwad V, Kapoor R, Thambudorai R. An ideal suture for midline abdominal closure? Indian J Surg. 2009;71(3):128-132.
doi pubmed - Jhobta RS, Attri AK, Kaushik R, Sharma R, Jhobta A. Spectrum of perforation peritonitis in India-review of 504 consecutive cases. World J Surg. 2006;7922:1-26.
- Malhotra MK, Singal R, Chowdhary K, Sharma RG, Sharma S, Dhankar A. Spectrum of perforation peritonitis in a Rural Medical College. Bangladesh J Med Sci. 2016;15(1):70-73.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
