| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Original Article
Volume 7, Number 4, December 2017, pages 58-63
Approach of the Bile Duct by Gastrostomy in Patients With Bypass in Roux-en-Y Proved to Be Safe and Effective
Luis Gustavo Santos Perissea, Paulo Cezar Marques Perissea, Trajano Salvador de Oliveira Filhoa, Idiberto Jose Zotarelli Filhob, c
aBariatric Surgery Department, Federal University of Rio de Janeiro, Rio de Janeiro (RJ), Brazil
bState University of Sao Paulo-Ibilce-Unesp, Rua Cristovao Colombo 2265, Sao Jose do Rio Preto (SP), Brazil
cCorresponding Author: Idiberto Jose Zotarelli Filho, University of Sao Paulo-Ibilce-Unesp, Rua Cristovao Colombo 2265, Sao Jose do Rio Preto (SP), Brazil
Manuscript submitted October 31, 2017, accepted December 15, 2017
Short title: Bile Duct via Gastrostomy With Roux-en-Y Bypass
doi: https://doi.org/10.14740/jcs336e
| Abstract | ▴Top |
Background: The prevalence and increase of obesity in the world are that 2.3 billion adults were overweight and 700 million adults were obese in 2015. In the context of the morbid obesity pandemic, bariatric surgery was presented as a gold standard treatment. It is known that the prevalence of cholelithiasis is 3 to 4 times higher in morbidly obese patients when compared to the general population. Literature reports that the first attempts to approach the biliary tract in patients with gastric bypass in Roux-en-Y, were performed transorally and had resulted in low success rates. The aim of this study was to analyze the results of the use of the endoscopic transgastrostomy technique for the treatment of biliary tract diseases in patients submitted to Y-de-Roux bypass.
Methods: Between August 2010 and December 2014, procedures of transgastrostomy endoscopic retrograde cholangiopancreatography (TG-ERCP) were performed in six patients, previously submitted to Roux-en-Y gastric bypass for treatment of morbid obesity.
Results: All patients were successfully submitted to procedures for duodenal papilla catheterization, cholangiography, and endoscopic papillotomy. No complications related to the surgical or endoscopic procedure were observed in the cases described, despite the small sample studied and also the variation of age and body mass index (BMI).
Conclusions: The technique described in the current study has been shown to be safe and effective. The possibility of performing it in single surgical time, as well as the use of conventional duodenoscopes and their accessories, make it a choice in patients undergoing Roux-en-Y gastric bypass.
Keywords: Transgastrostomy; Endoscopic retrograde cholangiopancreatography; Bile duct; Bypass gastric
| Introduction | ▴Top |
The prevalence and increase of obesity in the world are that 2.3 billion adults were overweight and 700 million adults were obese in 2015 [1, 2]. In Brazil, according to Brazilian Institute of Geography and Statistics, in the 34 years that have passed, the prevalence of overweight adults increased by almost three times in males (18.5% to 50.1%) and almost twice in women (from 28.7% to 48.0%) [3, 4]. In Europe, it is estimated that 10-20.0% of men and 15-25.0% of women are obese [5]. Moreover, in the USA, the prevalence of obesity is higher than 30% for both sexes, and obesity is the cause of death of 2.8 million people per year, affecting 26.0% of adults [5].
In the context of the morbid obesity pandemic, bariatric surgery was presented as a gold standard treatment. In 1994, Wittgrove et al [6] performed the first laparoscopic bypass in Roux-en-Y with the purpose of treating this pathology. This method, over the years, has become one of the most accomplished in the world [7], with about 140,000 procedures performed annually in the USA by the year 2008 [8].
It is known that the prevalence of cholelithiasis is 3 - 4 times higher in morbidly obese patients when compared to the general population, and that acute weight loss, such as that presented after the bypass in Roux-en-Y, predisposes to the appearance of gallstones [9]. Associating this fact with an increase in the number of patients submitted to this technique, a greater demand for interventions on the bile ducts is expected. In view of the anatomical changes determined by this surgery [10], the challenge of accessing the biliary tract in these patients is imposed on endoscopists.
Literature reports that the first attempts to approach the biliary tract in patients with gastric bypass in Roux-en-Y, in the reference center, were performed transorally with long front view equipment [11, 12]. These attempts, although conducted by experienced professionals, had resulted in low success rates. Therefore, the objective of the present study was to analyze the results of the use of the endoscopic transgastrostomy technique for the treatment of biliary tract diseases in patients submitted to Y-de-Roux bypass [12].
| Methods | ▴Top |
Between August 2010 and December 2014, procedures of TG-ERCP were performed in 6 patients, previously submitted to Roux-en-Y gastric bypass for treatment of morbid obesity (Table 1).
 Click to view | Table 1. Profile of Patients Studied and Clinical Outcome Obtained |
The procedures were performed in a surgical center, in a single surgical time, under general anesthesia, with the patient in dorsal decubitus position. General surgery teams were responsible for performing laparoscopic video gastrostomy on the portion of the stomach excluded from digestive transit (Fig. 1). The created gastrostomy was then readily used as an access route to approach the bile ducts, since that excluded stomach has continuity distally with the duodenum. A Fujinon duodenoscope, model ED 250 XT 5 was introduced through the gastrostomy performed (Fig. 2). Once in the stomach, the normal pathway via pylorus was used to reach the second duodenal portion. Catheterization of the duodenal papilla was then performed with the accessories normally used to perform transoral endoscopic cholangiopancreatography. All patients underwent cholangiography (C) with papillotomy (PAP). Bilateral prosthesis placement (BPP) was performed when necessary. At the end of the procedure the gastrostomy was closed with direct or maintained suture in the case of need for a new approach of the bile duct.
 Click for large image | Figure 1. Gastrostomy fixed to the skin. |
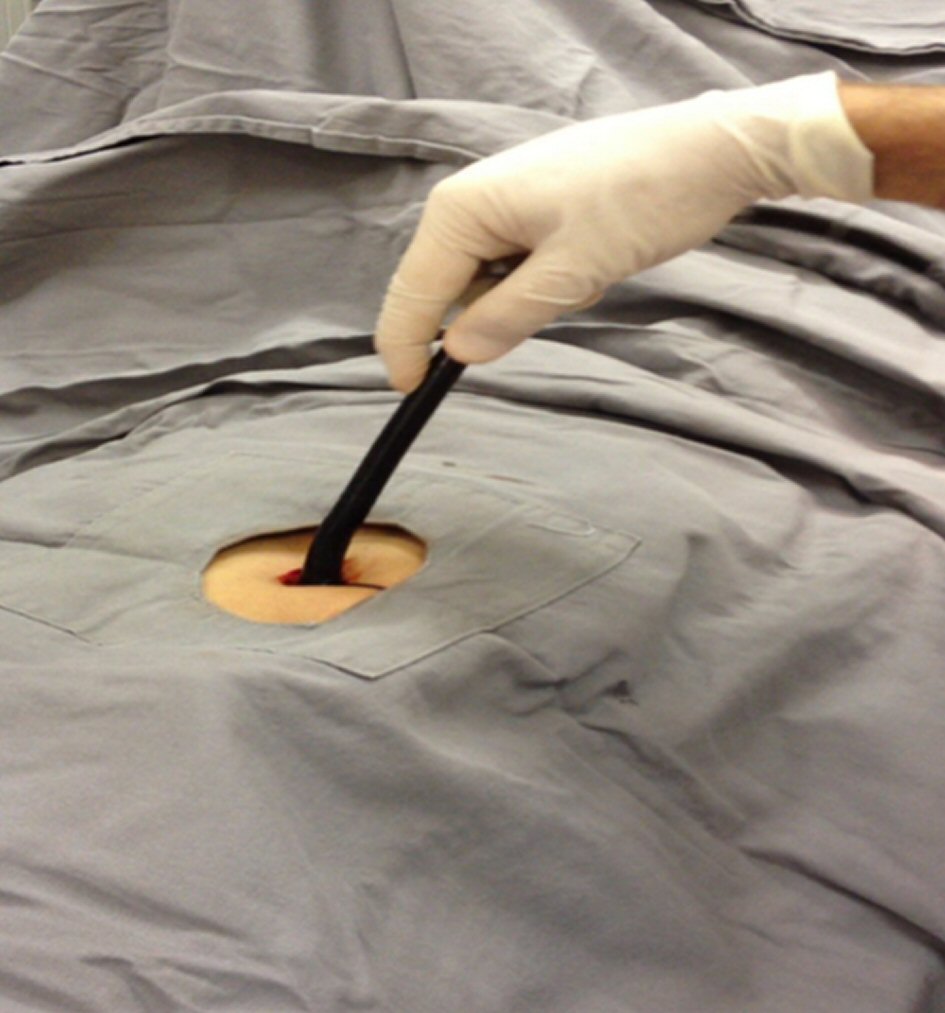 Click for large image | Figure 2. Introduction of the duodenoscope. |
Primary outcome
To analyze the safety of the use of endoscopic transgastrostomy approach in single surgical time as well as the use of conventional duodenoscopes and their accessories for the treatment of biliary tract diseases in patients submitted to Y-de-Roux bypass.
Secondary outcome
To analyze the success of using the technique of endoscopic transgastrostomy approach, in a single surgical time.
| Results | ▴Top |
All patients in the present study were female, ranging in age from 22 to 47 years, mean age of 35 years, preoperative body mass index (BMI) between 40.5 and 47.7 kg/m2, mean of 42.5 kg/m2. All patients underwent Roux-en-Y derivation for obesity treatment. In five patients the indication for ERCP was choledocholithiasis (CL). In the remaining patient (patient 1), the procedure was indicated for main treatment of lesion bile duct (LBD). The hospital stay lasted from 2 to 10 days, with a mean of 4.17 days.
All patients were successfully submitted to procedures for duodenal papilla catheterization, cholangiography, and endoscopic papillotomy. In patients numbers 3, 5 and 6, immediately after performing ERCP, laparoscopic cholecystectomy (LCL) was performed at the same time. In the patient number 1, the position of plastic bile prosthesis (PBP) for treatment of primary bile duct injury (BDI) was chosen, and gastrostomy was maintained due to the need for a new procedure to remove the bile duct. The patient was discharged 10 days after the placement of the bile duct, and was later readmitted for its removal, being discharged 2 days later. In the other patients, the ostomy was closed immediately after the endoscopic procedure. Two patients remained in hospital for more than 2 days because they needed clinical follow-up unrelated to the procedure (patient 1) and antibiotic therapy to treat acute cholecystitis (patient 6).
No complications related to the surgical or endoscopic procedure were observed in the cases described.
| Discussion | ▴Top |
The increased prevalence of obesity is well described in the medical literature [4]. In 2010, the number of bariatric surgeries performed in the USA exceeded 150,000 cases annually, with the second abdominal surgery being the most commonly performed, with 60.0% of the cases corresponding to Y-de-Roux leads [13]. With the large number of surgical procedures performed to treat obesity and the known increase in gallstone formation associated with acute weight loss [14], a significant increase in the need for ERCP in these patients is to be expected. The presence of a Y-de-Roux with long handles, made for weight loss, makes the examination even more difficult [15].
Attempts to use conventional duodenoscopes per-orally to approach these patients were not encouraging. Hintze et al [16] reported unsatisfactory results in the treatment of patients with non-obesity-related Roux-en Y, with failure rates of 67.0%, mainly due to inability to reach the papilla.
As an alternative to the use of oral duodenoscopes, several techniques have been developed, involving the use of frontal and longer vision devices [15]. Standard enteroscopy (using pediatric and enteroscopic colonoscopes) and deep one (balloon, double balloon, or spiral) help the endoscopist to overcome the challenge of transposing long segments of the small intestine and reaching the duodenal papilla. However, new problems arise with the use of such equipment. The reduced number of compatible accessories, the approach and catheterization of the papilla with frontal view device, without forceps lift, as well as the retrograde approach of the papilla should be considered as factors that add difficulty and limit the success rates obtained with these techniques [15, 17].
In this context, success rates of papillary or bile anastomosis range 55.0-100.0% in the series described in the literature, with catheterization rates, after reaching, above 90.0% [18-31], no identified significant difference between methods [28]. The high success rates of both papillary reach and bile duct catheterization should be attributed to the fact that most of the patients reported were not carriers of Roux-en-Y made with the purpose of weight loss, thus presenting segments of intestinal loops that make up the Y shorter, when compared to patients after bariatric surgery. Another determining factor in obtaining high success rates of papilla catheterization was the presence of digestive bile anastomoses instead of the native papilla in most patients [18-31]. Increased complication rates in these procedures, including perforation and pancreatitis, have also been reported [15, 20, 26, 30, 32, 33]. Furthermore, Schapira et al [34] described in 1975 the implementation of ERCP by means of preexisting gastrostomy for the evaluation of obstructive pattern jaundice. Subsequent reports demonstrated the efficacy of the method [35, 36].
In 1998, access was made for the first time by gastrostomy exclusively made for this purpose [37], in a patient with Roux-en-Y for the treatment of obesity. Subsequent studies reaffirmed the feasibility and efficacy of the procedure, with success rates varying from 97% to 100% when considering papilla catheterization and post-catheterization interventions [38-42]. The possibility of access to the bile duct by means of the creation of an ostomy, by means of laparoscopic or percutaneous puncture (through the use of interventional radiology techniques), in the excluded part of the stomach, allows the use of a duodenoscope in a conventional way, allowing the unrestricted use of accessories to perform ERCP. The time required for the maturation of gastrostomy for subsequent endoscopic procedure is shown as the main disadvantage of the method, making it impossible to use the technique in emergency and emergency situations [15].
Laparoscopically assisted ERCP has been gaining popularity in recent years, which may be evidenced by case reports and small published series [15]. Unlike transgastrostomy access, in which the surgical and endoscopic procedures are performed at operative times, distinct laparoscopically assisted ERCP allows the procedures to be performed at the same surgical time, and it is possible to perform them in cases of urgency [15]. Patients are assisted by surgery and endoscopy teams. After laparoscopic access to the abdominal cavity, the excluded portion of the stomach is individualized and gastrotomy is performed.
Still under laparoscopic vision and with the surgeon’s help, the duodenoscope, previously sterilized through the use of ethylene oxide, is introduced into the abdominal cavity through the laparoscopic trocar, and later into the gastric orifice having access to the pylorus and second duodenal portion. Case series described in the literature point to success rates up to 100.0%, with complication rates similar to the traditional procedure [10, 43-47], demonstrating that it is technically superior to those using long frontal vision devices.
The need for prior sterilization of the duodenoscope instead of the use of high level disinfection, normally used and available in the endoscopy units, the limitation of movement imposed on the endoscopist by the presence of the trochlee involving the endoscope as well as the mandatory presence of the surgical team throughout the procedure are important factors that limit the diffusion of the use of this technique [10, 43-47].
In the present study all procedures were performed in patients undergoing gastric bypass at Y-de-Roux for treatment of morbid obesity thus presenting longer Y-loops. All procedures were performed in single surgical time, as described by Pimentel et al in 2004 [38], in an isolated case report. The creation of gastrostomy in the excluded portion of the stomach eliminates the obstacles created by the distance to be traveled by the device to the papilla, allowing the use of traditional duodenoscopes safely.
The possibility of using accessories compatible with the duodenoscope, the presence of the elevator, as well as the approach of the papilla in conventional position make the procedure efficient and safe. The success rates obtained in the present study are similar to those described for the conventional method, for per-oral route; being superior to those obtained with the use of frontal vision devices [18, 19-31].
When compared to procedures that somehow combine the use of duodenoscope and transgastric access to the bile duct [10, 38-47] the method of the present study presents important advantages. Because it is performed in a single surgical time, without having to wait for the gastrostomy maturation, different from other reports of gastrostomy use [35-37, 39-42], its use is adequate in the emergency scenarios, making its application more comprehensive. When compared to laparoscopically assisted procedures [10, 43-47], the absence of trocars involving the duodenoscope allows the endoscopist to perform a greater range of movements, thus reducing the difficulty of performing the exam.
The fact that none of the patients presented complications, related to the surgical or endoscopic act, points to a safety scenario of the method, despite the small sample studied and also the variation of age and BMI.
The main limitation of the present study was the small casuistry.
Conclusions
The technique described in the current study has been shown to be safe and effective. The possibility of performing it in single surgical time, as well as the use of conventional duodenoscopes and their accessories, make it a choice in patients undergoing Roux-en-Y gastric bypass.
| References | ▴Top |
- Al-Zubaidi AM, Alghamdi HU, Alzobydi AH, Dhiloon IA, Qureshi LA. Bowel perforation due to break and distal passage of the safety ring of an adjustable intra-gastric balloon: A potentially life threatening situation. World J Gastrointest Endosc. 2015;7(4):429-432.
doi pubmed - Al-Sabah S, Al-Ghareeb F, Ali DA, Al-Adwani A. Efficacy of intragastric balloon for the management of obesity: experience from Kuwait. Surg Endosc. 2016;30(2):424-429.
doi pubmed - IBGE- Instituto Brasileiro de Geografia e Estatistica. Disponivel em: http://www.ibge.gov.br. Acesso em marco de 2015.
- Nguyen DM, El-Serag HB. The big burden of obesity. Gastrointest Endosc. 2009;70(4):752-757.
doi pubmed - WHO- World Health Organization. Disponivel em: Acesso em: 30 de marco de 2015.
- Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes Surg. 1994;4(4):353-357.
doi pubmed - Nguyen NT, Root J, Zainabadi K, Sabio A, Chalifoux S, Stevens CM, Mavandadi S, et al. Accelerated growth of bariatric surgery with the introduction of minimally invasive surgery. Arch Surg. 2005;140(12):1198-1202; discussion 1203.
doi pubmed - Buchwald H, Oien DM. Metabolic/bariatric surgery Worldwide 2008. Obes Surg. 2009;19(12):1605-1611.
doi pubmed - Wattchow DA, Hall JC, Whiting MJ, Bradley B, Iannos J, Watts JM. Prevalence and treatment of gall stones after gastric bypass surgery for morbid obesity. Br Med J (Clin Res Ed). 1983;286(6367):763.
doi - Falcao M, Campos JM, Galvao Neto M, Ramos A, Secchi T, Alves E, Franca E, et al. Transgastric endoscopic retrograde cholangiopancreatography for the management of biliary tract disease after Roux-en-Y gastric bypass treatment for obesity. Obes Surg. 2012;22(6):872-876.
doi pubmed - Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53(2):216-220.
doi pubmed - Sakai P, Kuga R, Safatle-Ribeiro AV, Faintuch J, Gama-Rodrigues JJ, Ishida RK, Furuya CK, Jr., et al. Is it feasible to reach the bypassed stomach after Roux-en-Y gastric bypass for morbid obesity? The use of the double-balloon enteroscope. Endoscopy. 2005;37(6):566-569.
doi pubmed - Birkmeyer NJ, Dimick JB, Share D, Hawasli A, English WJ, Genaw J, Finks JF, et al. Hospital complication rates with bariatric surgery in Michigan. JAMA. 2010;304(4):435-442.
doi pubmed - Shiffman ML, Sugerman HJ, Kellum JM, Brewer WH, Moore EW. Gallstone formation after rapid weight loss: a prospective study in patients undergoing gastric bypass surgery for treatment of morbid obesity. Am J Gastroenterol. 1991;86(8):1000-1005.
pubmed - Lee A, Shah JN. Endoscopic approach to the bile duct in the patient with surgically altered anatomy. Gastrointest Endosc Clin N Am. 2013;23(2):483-504.
doi pubmed - Hintze RE, Adler A, Veltzke W, Abou-Rebyeh H. Endoscopic access to the papilla of Vater for endoscopic retrograde cholangiopancreatography in patients with billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29(2):69-73.
doi pubmed - Khashab MA, Okolo PI, 3rd. Accessing the pancreatobiliary limb and ERCP in the bariatric patient. Gastrointest Endosc Clin N Am. 2011;21(2):305-313.
doi pubmed - Elton E, Hanson BL, Qaseem T, Howell DA. Diagnostic and therapeutic ERCP using an enteroscope and a pediatric colonoscope in long-limb surgical bypass patients. Gastrointest Endosc. 1998;47(1):62-67.
doi - Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39(12):1068-1071.
doi pubmed - Raithel M, Dormann H, Naegel A, Boxberger F, Hahn EG, Neurath MF, Maiss J. Double-balloon-enteroscopy-based endoscopic retrograde cholangiopancreatography in post-surgical patients. World J Gastroenterol. 2011;17(18):2302-2314.
doi pubmed - Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointest Endosc. 2007;66(5):1038-1041.
doi pubmed - Parlak E, Cicek B, Disibeyaz S, Cengiz C, Yurdakul M, Akdogan M, Kilic MZ, et al. Endoscopic retrograde cholangiography by double balloon enteroscopy in patients with Roux-en-Y hepaticojejunostomy. Surg Endosc. 2010;24(2):466-470.
doi pubmed - Neumann H, Fry LC, Meyer F, Malfertheiner P, Monkemuller K. Endoscopic retrograde cholangiopancreatography using the single balloon enteroscope technique in patients with Roux-en-Y anastomosis. Digestion. 2009;80(1):52-57.
doi pubmed - Wang AY, Sauer BG, Behm BW, Ramanath M, Cox DG, Ellen KL, Shami VM, et al. Single-balloon enteroscopy effectively enables diagnostic and therapeutic retrograde cholangiography in patients with surgically altered anatomy. Gastrointest Endosc. 2010;71(3):641-649.
doi pubmed - Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, et al. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol. 2010;105(1):93-99.
doi pubmed - Saleem A, Baron TH, Gostout CJ, Topazian MD, Levy MJ, Petersen BT, Wong Kee Song LM. Endoscopic retrograde cholangiopancreatography using a single-balloon enteroscope in patients with altered Roux-en-Y anatomy. Endoscopy. 2010;42(8):656-660.
doi pubmed - Shah RJ, Smolkin M, Yen R, Ross A, Kozarek RA, Howell DA, Bakis G, et al. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc. 2013;77(4):593-600.
doi pubmed - Shimatani M, Matsushita M, Takaoka M, Koyabu M, Ikeura T, Kato K, Fukui T, et al. Effective "short" double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41(10):849-854.
doi pubmed - Cho S, Kamalaporn P, Kandel G, Kortan P, Marcon N, May G. ‘Short’ double-balloon enteroscope endoscopic retrograde cholangiopancreatography in patients with a surgically altered upper gastrointestinal tract. Can J Gastroenterol. 2011;25(11):615-619.
doi pubmed - Siddiqui AA, Chaaya A, Shelton C, Marmion J, Kowalski TE, Loren DE, Heller SJ, et al. Utility of the short double-balloon enteroscope to perform pancreaticobiliary interventions in patients with surgically altered anatomy in a US multicenter study. Dig Dis Sci. 2013;58(3):858-864.
doi pubmed - Wagh MS, Draganov PV. Prospective evaluation of spiral overtube-assisted ERCP in patients with surgically altered anatomy. Gastrointest Endosc. 2012;76(2):439-443.
doi pubmed - Gerson LB, Tokar J, Chiorean M, Lo S, Decker GA, Cave D, Bouhaidar D, et al. Complications associated with double balloon enteroscopy at nine US centers. Clin Gastroenterol Hepatol. 2009;7(11):1177-1182, e1171-1173.
- Lennon AM, Kapoor S, Khashab M, Corless E, Amateau S, Dunbar K, Chandrasekhara V, et al. Spiral assisted ERCP is equivalent to single balloon assisted ERCP in patients with Roux-en-Y anatomy. Dig Dis Sci. 2012;57(5):1391-1398.
doi pubmed - Schapira L, Falkenstein DB, Zimmon DS. Endoscopy and retrograde cholangiography via gastrostomy. Gastrointest Endosc. 1975;22(2):103.
doi - Gray R, Leong S, Marcon N, Haber G. Endoscopic retrograde cholangiography, sphincterotomy, and gallstone extraction via gastrostomy. Gastrointest Endosc. 1992;38(6):731-732.
doi - Holderman WH, Etzkorn KP, Harig JM, Watkins JL. Endoscopic retrograde cholangiopancreatography and stent placement via gastrostomy: technical aspects and clinical application. Endoscopy. 1995;27(1):135-137.
doi pubmed - Baron TH, Vickers SM. Surgical gastrostomy placement as access for diagnostic and therapeutic ERCP. Gastrointest Endosc. 1998;48(6):640-641.
doi - Pimentel RR, Mehran A, Szomstein S, Rosenthal R. Laparoscopy-assisted transgastrostomy ERCP after bariatric surgery: case report of a novel approach. Gastrointest Endosc. 2004;59(2):325-328.
doi - Matlock J, Ikramuddin S, Lederer H, Cass O. Bypassing the bypass: ERCP via gastrostomy after bariatric surgery. Gastointest Endosc. 2005;61:AB98.
doi - Gutierrez JM, Lederer H, Krook JC, Kinney TP, Freeman ML, Jensen EH. Surgical gastrostomy for pancreatobiliary and duodenal access following Roux en Y gastric bypass. J Gastrointest Surg. 2009;13(12):2170-2175.
doi pubmed - Tekola B, Wang AY, Ramanath M, Burnette B, Ellen K, Schirmer BD, Hallowell PT, et al. Percutaneous gastrostomy tube placement to perform transgastrostomy endoscopic retrograde cholangiopancreaticography in patients with Roux-en-Y anatomy. Dig Dis Sci. 2011;56(11):3364-3369.
doi pubmed - Choi EK, Chiorean MV, Cote GA, El H, II, Ballard D, Fogel EL, Watkins JL, et al. ERCP via gastrostomy vs. double balloon enteroscopy in patients with prior bariatric Roux-en-Y gastric bypass surgery. Surg Endosc. 2013;27(8):2894-2899.
doi pubmed - Lopes TL, Clements RH, Wilcox CM. Laparoscopy-assisted ERCP: experience of a high-volume bariatric surgery center (with video). Gastrointest Endosc. 2009;70(6):1254-1259.
doi pubmed - Bertin PM, Singh K, Arregui ME. Laparoscopic transgastric endoscopic retrograde cholangiopancreatography (ERCP) after gastric bypass: case series and a description of technique. Surg Endosc. 2011;25(8):2592-2596.
doi pubmed - Vilallonga R, Pimentel R, Rosenthal RJ. Hybrid endolaparoscopic management of biliary tract pathology in bariatric patients after gastric bypass: case report and review of a single-institution experience. Surg Laparosc Endosc Percutan Tech. 2013;23(5):e188-190.
doi pubmed - Saleem A, Levy MJ, Petersen BT, Que FG, Baron TH. Laparoscopic assisted ERCP in Roux-en-Y gastric bypass (RYGB) surgery patients. J Gastrointest Surg. 2012;16(1):203-208.
doi pubmed - Schreiner MA, Chang L, Gluck M, Irani S, Gan SI, Brandabur JJ, Thirlby R, et al. Laparoscopy-assisted versus balloon enteroscopy-assisted ERCP in bariatric post-Roux-en-Y gastric bypass patients. Gastrointest Endosc. 2012;75(4):748-756.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
