| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Case Report
Volume 4, Number 3, September 2014, pages 95-98
Hematemesis From a Left Gastric Artery Pseudoaneurysm Secondary to an Adjustable Laparoscopic Gastric Band
Eric Downesa, Kristen Bakera, Jessica L. Buickob, e, Kandace M. Kichlerb, Lawrence H. Brickmana, Miguel A. Lopez-Viegoc, d
aFlorida Atlantic University School of Medicine, Boca Raton, FL, USA
bUniversity of Miami Palm Beach Regional Campus, Atlantis, FL, USA
cDepartment of General and Vascular Surgery, JFK Medical Center, Atlantis, FL, USA
dBethesda Memorial Hospital, Boynton Beach, FL, USA
eCorresponding Author: Jessica L. Buicko, University of Miami, JFK Medical Center, Atlantis, FL, USA
Manuscript accepted for publication July 23, 2014
Short title: Left Gastric Artery Pseudoaneurysm
doi: https://doi.org/10.14740/jcs234w
| Abstract | ▴Top |
Gastric band erosion into the lumen of the stomach or the esophagus is a fairly common but often underreported complication of laparoscopic adjustable gastric banding surgery. It occurs in as many as 3-11% of patients who undergo the procedure. We present here the case of a 56-year-old morbidly obese female who developed the sudden onset of hematemesis and dysphagia more than 3 years after laparoscopic gastric band placement. Endoscopy was performed at presentation and revealed erosion into the proximal gastric lumen. The patient was stabilized with medical management of her anemia and abdominal pain. Both the band and subcutaneous reservoir were subsequently removed laparoscopically. A perforation of the gastric wall was identified and treated with a falciform ligament patch and naso-gastric decompression. Five days after surgical band removal, the patient had an episode of hematemesis productive of over 750 cc of blood, accompanied by tachycardia and hypotension. Mesenteric (celiac artery) angiography revealed an actively bleeding pseudoaneurysm of the left gastric artery that was successfully thrombosed with coils. The patient was kept nil per os (NPO) on total parenteral nutrition (TPN) for 1 week postoperatively and remained stable. A follow-up gastrograffin upper gastrointestinal (GI) study showed no leak from the perforation site. To our knowledge, this is the first reported case in which an erosion from an adjustable laparoscopic gastric band was associated with massive upper GI bleeding from a left gastric artery pseudoaneurysm. The case demonstrates the importance of monitoring a patient with hematemesis post lap band surgery, as life-threatening bleeding may persist after removal of the gastric band.
Keywords: Pseudoaneurysm; Gastric band; Laparoscopy; Bariatric surgery
| Introduction | ▴Top |
According to the Centers for Disease Control, more than one-third of US adults are obese (defined as a body mass index (BMI) of 30 or greater) [1]. The estimated annual medical cost of obesity is $147 billion in US dollars with individual medical costs $1,429 higher on average for the obese adult [2]. Weight loss through lifestyle modification is first-line treatment for obesity. In these patients, as little as 5% weight loss has been shown to improve glycemic control and reduce incidence of type II diabetes [3]. In cases in which conservative management fails, however, bariatric surgery remains a viable alternative for reducing BMI. At least one randomized control trial demonstrated greater weight loss from bariatric surgery vs. lifestyle modification after 2 years of treatment [4]. Laparoscopic adjustable gastric banding (LAGB) surgery is perhaps the most popular procedure worldwide accounting for more than 40% of all bariatric surgeries in 2008. Benefits of this surgery include lower complication rates, reversibility and minimal invasiveness [5]. Morbidity rates for LAGB surgery vary widely from study to study, perhaps due to different definitions of adverse events. A 2002 systematic review of LAGB surgery by the Royal Australian College of Surgeons reported a median morbidity rate of 10.7% (range of 0-68% over 34 studies) vs. 23.6% for vertical banded gastroplasty and 27.4% for Roux-En-Y surgery [6]. Examples of complications of LAGB include leakage of the balloon, band or port site infections, esophageal dilations leading to dysphagia, band migration along stomach and gastroesophageal junction, and band erosion into stomach leading to infections and the gastrointestinal (GI) hemorrhage [7].
Here we report a 56-year-old female with recurrent hematemesis refractory to band removal due to a left gastric artery pseudoaneurysm associated with a band erosion into the stomach.
| Case Report | ▴Top |
Patient K.M. was a 56-year-old female with a past medical history significant for morbid obesity, hypertension, type II diabetes mellitus, chronic anemia, and LAGB surgery in 2010 who presented to our hospital’s emergency room complaining of three to four episodes of hematemesis, all during the previous 24 h. For the past 3 months prior to admission, she related that she experienced dysphagia when ingesting solid foods associated with postprandial vomiting. She reported episodes of frequently regurgitating undigested food. She denied abdominal pain or changes in bowel habits. Of note, she had not had any adjustments (fills) to her lap gastric band since insertion (placed at a different facility). She denied smoking, alcohol or any illicit drug use. In the emergency room, her vitals were stable. Her calculated BMI was 43.07. Other than morbid obesity, the patient’s physical examination was unremarkable. A complete blood count revealed a normocytic anemia with a hemoglobin of 11.1 g/dL (reference range 12.0 - 16.0 g/dL) and a hematocrit of 34.0% (reference range of 37.0-47.0%). A complete metabolic panel was remarkable for glucose of 171 mg/dL; her liver function panel was unremarkable except for a serum albumin of 2.9 g/dL (reference range 3.4 - 5.0 g/dL). Serum lipase was within normal limits. An upright AP film of the chest was normal. The source of her bleeding was determined to be in the upper GI tract, and the patient was kept overnight on an intravenous (IV) protonix drip in the hospital to await gastroenterology consultation and evaluation. An endoscopy performed the following day revealed an obstructing foreign body resembling the lap gastric band in the distal esophagus and proximal stomach (Fig. 1). The scope was passed beyond the obstruction where old and fresh blood was noted in the distal stomach and duodenum. The patient was then transferred to the intensive care unit (ICU) and a surgical consultation was obtained. Our surgical team scheduled the patient for laparoscopic removal of the adjustable gastric band on the following morning. In the meantime, a computer tomography (CT) scan of the abdomen and pelvis without contrast revealed circumferential air bubbles adjacent the lab band within the gastric cardia (Fig. 2). Prior to surgery, the patient’s vitals remained stable. Her hemoglobin/hematocrit (H/H) were 10.0 g/dL and 31.6%. The patient’s leukocyte count was consistently in reference range (45,000 - 110,000/µL) prior to operation. During the operative procedure, the lap gastric band appeared grossly infected and was noted to be encased in a foul-smelling discharge. A naso-gastric tube placed into the stomach by the anesthesia team intraoperatively demonstrated perforation of the band into the lumen of the stomach. The gastric perforation was identified and patched using the falciform ligament. The remainder of the laparoscopic exploration was unremarkable and thepatient was taken to the ICU in stable condition. The patient was kept nil per os (NPO) postoperatively, and total parenteral nutrition (TPN) was administered along with broad-spectrum IV antibiotics. The wound culture grew Escherichia coli, Enterococcus and Proteus mirabilis, and the patient’s antibiotic regimen was changed to imipenem/cilastin. On postoperative day 1 the patient was doing well. The patient’s H/H, however, did not return to reference levels. On postoperative day 5, the patient coughed up 750 cc bright red blood and was tachycardic with a peak heart rate of 155 bpm. Her H/H were found to be 7.01 g/dL and 21.4%. Subcutaneous administration of heparin for deep venous thrombosis prophylaxis was stopped. She was given three units packed red blood cells and her H/H rose to 9.21 g/dL and 27.8%. She then underwent angiography where a pseudoaneurysm was noted in the left gastric artery (Fig. 3). A 5 mm × 6 cm hydrogel coil as well as several 5 and 7 mm fibered coils were used to occlude the left gastric artery proximally and the pseudoaneurysm distally. A postprocedure angiogram showed successful occlusion of left gastric artery. After pseudoaneurysm and left gastric artery embolization, the patient’s H/H and vitals remained stable. She was successful weaned from TPN and advanced to a bariatric diet in the outpatient setting.
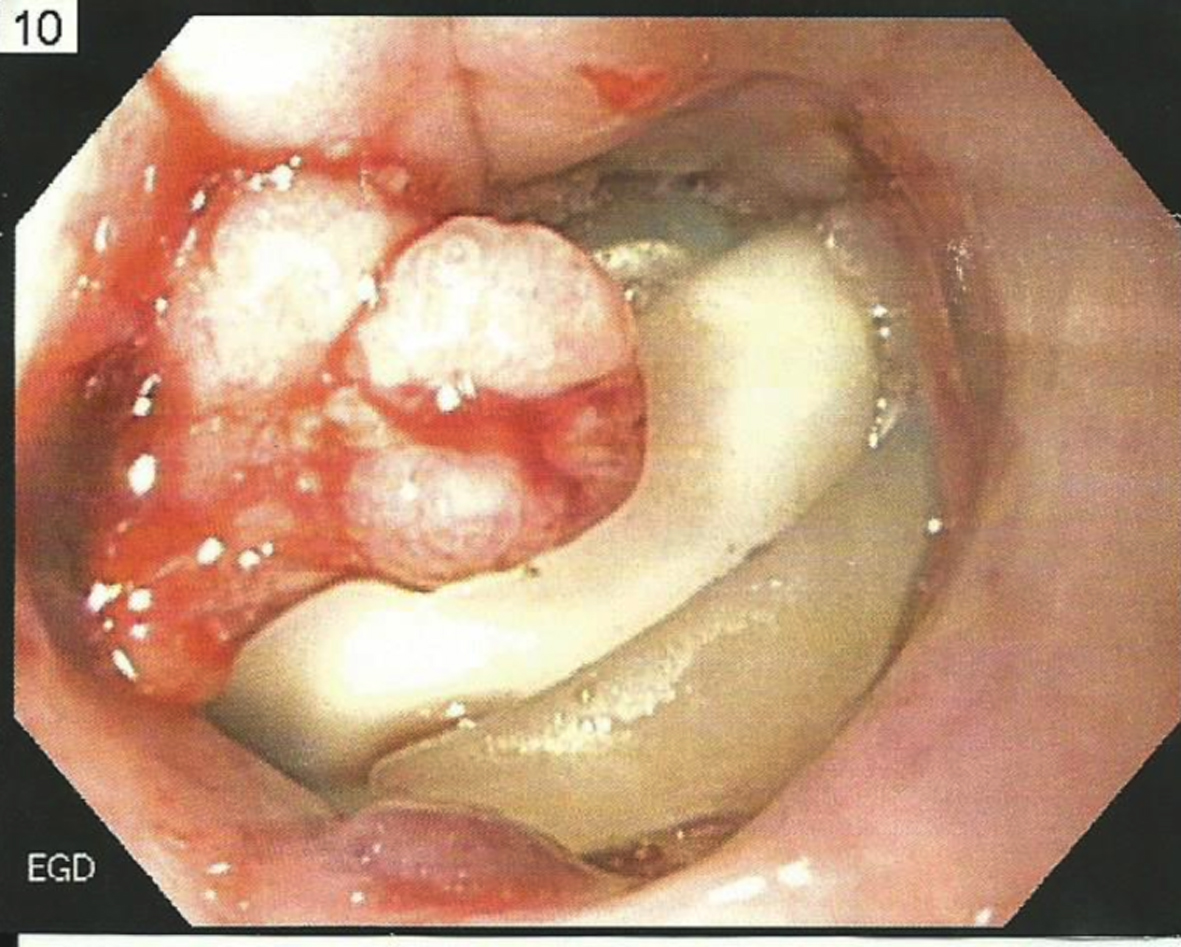 Click for large image | Figure 1. Endoscopic image revealing erosion of lap band into proximal gastric lumen. |
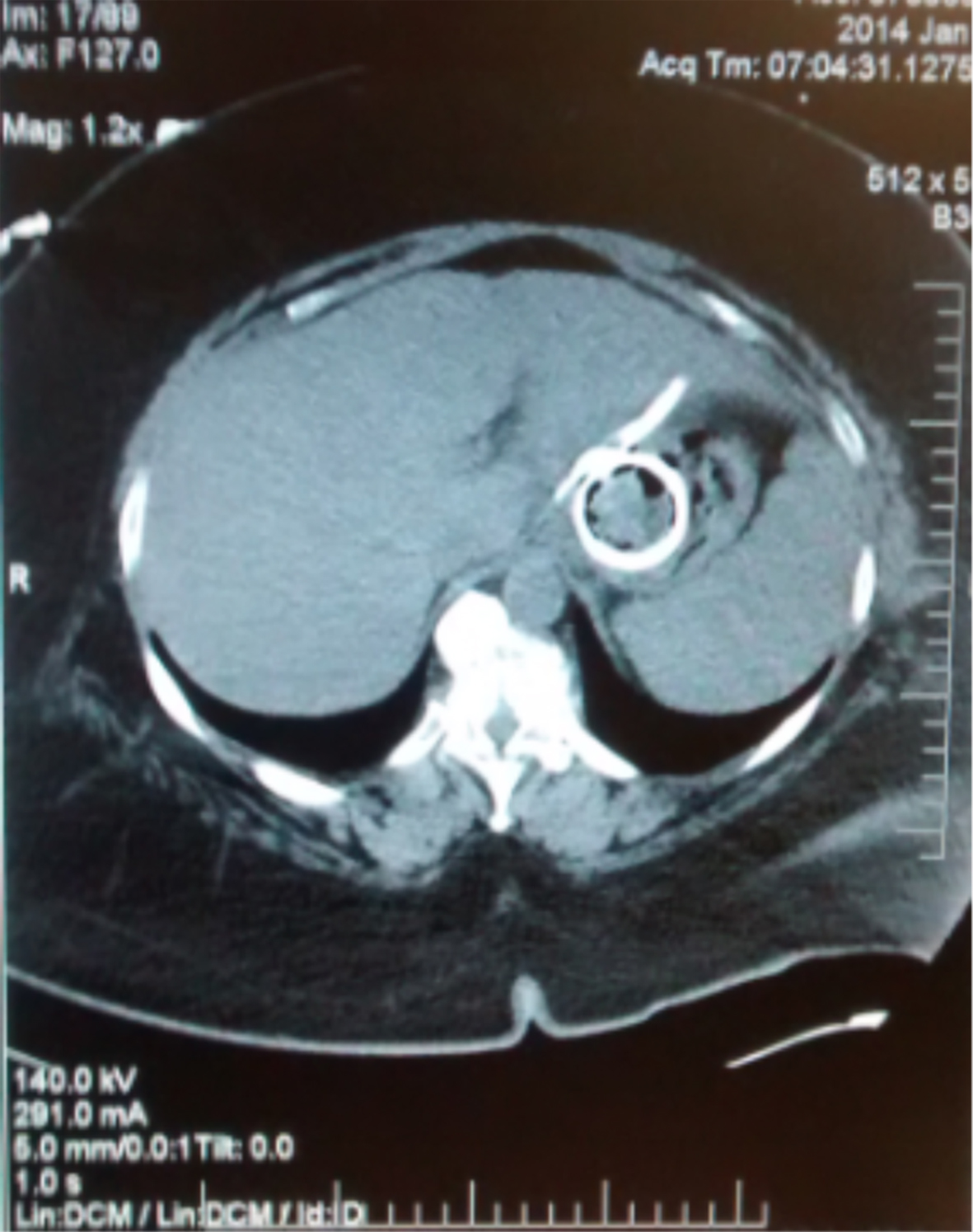 Click for large image | Figure 2. CT of abdomen showing an unusual distribution of small gas bubbles adjacent to the loop of the lap band in the gastric cardia suggestive of pneumatosis in the gastric wall. |
 Click for large image | Figure 3. Mesenteric angiography demonstrating an irregular pseudoaneurysm with contained extravasation involving the left gastric artery. Of note, the left gastric artery was subsequently successfully occluded proximal and distal to the pseudoaneurysm using hydrogel and fibered microcoils. |
| Discussion | ▴Top |
Gastric band erosion is a relatively common, long-term complication (> 6 months) of LAGB surgery associated with weight regain, chronic port-cutaneous fistulas, protracted port site infections, insidious peritonitis, subphrenic abcesses and GI bleeding, but the exact etiology of band erosion is unclear [8, 9]. Chronic ischemia due to pressure on gastric wall by the device, chronic inflammation of tissue adjacent to the band or weakening of gastric wall due to intraoperative gastric wall trauma may all contribute the gastric band migration leading to erosion [9, 10]. Erosion itself, moreover, does not always involve the stomach or the band itself. Cintolo et al reported a patient with erosion of the gastric band into the duodenum with reported port side infections [5]. Epigastric pain is the most common symptom of intragastric migration [10]. This complication is not usually life-threatening. For patients presenting with melena, endoscopy provides the initial study of choice and is usually sufficient for diagnosis. However, in a patient with an acute or serious bleed, especially in the setting of hypotension, such a technique may not reveal the site of bleeding [10]. Diagnosis of a celiac axis erosion in a 49-year-old female with LAGB could not be made via endoscopy alone; an urgent laparotomy finally revealed the location of erosion [11]. In patients presenting with other symptoms such as abdominal pain and port site infections, CT scans and upper GI series provided the means of diagnosis. CT has the added benefit of having the ability to evaluate the erosion of tubing into other structures within the peritoneum and to assess for pneumoperitoneum or asymptomatic intraabdominal abcess [5, 8]. Screening patients with CT and upper GI series after lap band surgery has the potential to prevent the development of full-fledged erosion, as chronic band migration and abscesses may be asymptomatic [8, 11].
Our patient, like many other patients reported in the literature, initially met weight loss goals and did not become symptomatic until years after LAGB placement. She was aggressively treated with laparoscopic removal of the gastric band scheduled soon after her diagnosis. Torab et al attempted to treat a 38-year-old female with epigastric pain, dizziness, fainting and melena conservatively until a time in which the band could be removed via endoscope. After 1 year, the pain became intolerable for the patient, ultimately resulting in laparoscopic removal of the band [10]. Since our patient already suffered from chronic anemia and because the band appeared grossly infected during laparoscopy, aggressive management was chosen. Her continued bleeding post-laparoscopy provided a diagnostic dilemma. A repeat endoscopy with insufflation of air was not preferable secondary to the gastric perforation that was demonstrated during the initial surgery. Angiography provided the best option for our patient who had normal renal function. To our knowledge, this is the first reported case in which an eroded lap band has been shown to cause a pseudoaneurysm of the left gastric artery and acute severe GI bleeding. This case highlights an important potential complication of LAGB surgery and its management.
| References | ▴Top |
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009-2010. NCHS data brief, no 82. Hyattsville, MD: National Center for Health Statistics. 2012.
- Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood). 2009;28(5):w822-831.
doi pubmed - Klein S, Sheard NF, Pi-Sunyer X, Daly A, Wylie-Rosett J, Kulkarni K, Clark NG. Weight management through lifestyle modification for the prevention and management of type 2 diabetes: rationale and strategies: a statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical Nutrition. Diabetes Care. 2004;27(8):2067-2073.
doi pubmed - O'Brien PE, Dixon JB, Laurie C, Skinner S, Proietto J, McNeil J, Strauss B, et al. Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomized trial. Ann Intern Med. 2006;144(9):625-633.
doi pubmed - Cintolo JA, Levine MS, Huang S, Dumon K. Intraluminal erosion of laparoscopic gastric band tubing into duodenum with recurrent port-site infections. J Laparoendosc Adv Surg Tech A. 2012;22(6):591-594.
doi pubmed - Chapman A, Foster B, Game P, Ham J, Kiroff G, Maddern G, et al. Systematic review of laparoscopic adjustable gastric banding for the treatment of obesity: Update and re-appraisal. ASERNIP-S Report No. 31, Second Edition. Adelaide, South Australia: ASERNIP-S, June 2002.
- Klein S, Fabbrini E, Romijin JA. Obesity. In: Melmed S, Polonsky KS, Larsen PR, Kronenberg HM, eds. Melmed: Williams Textbook of Endocrinology, 12th ed. Philadelphia: Saunders, An Imprint of Elsevier Inc.; 2011:1642.
- Wylezol M, Sitkiewicz T, Gluck M, Zubik R, Pardela M. Intra-abdominal abscess in the course of intragastric migration of an adjustable gastric band: a potentially life-threatening complication. Obes Surg. 2006;16(1):102-104.
doi pubmed - Rao AD, Ramalingam G. Exsanguinating hemorrhage following gastric erosion after laparoscopic adjustable gastric banding. Obes Surg. 2006;16(12):1675-1678.
doi pubmed - Torab FC, Hefny AF, Taha M, Abou-Rebyeh H, Abu-Zidan FM. Delayed life-threatening upper gastrointestinal bleeding as a complication of laparoscopic adjustable gastric banding: case report and review of the literature. Asian J Surg. 2012;35(3):127-130.
doi pubmed - Iqbal M, Manjunath S, Seenath M, Khan A. Massive upper gastrointestinal hemorrhage: an unusual presentation after laparoscopic adjustable gastric banding due to erosion into the celiac axis. Obes Surg. 2008;18(6):759-760.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
