| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org/ |
Original Article
Volume 6, Number 1, March 2016, pages 21-29
Length of Hospitalization: A Protective Factor in a Prospective Observational Cohort Study in Brazilian ASA III and IV Hip Fracture Elderly Patients
Tiango Aguiar Ribeiroa, b, c, f, Ricardo Issler Unfriedc, Luiz Giulian Britoc, Klaus de Souza Steinc, Joao Alberto Larangeirac, Odirlei Andre Monticielod, e
aPost-Graduate Program of Health Science, Federal University of Santa Maria (UFSM), Santa Maria, Rio Grande do Sul, Brazil
bDepartment of Surgery in Orthopaedic, Medicine School of Federal University of Santa Maria (UFSM), Santa Maria, Rio Grande do Sul, Brazil
cDepartment of Orthopaedic, University Hospital of Santa Maria (SOT-HUSM), Federal University of Santa Maria (UFSM), Santa Maria, Rio Grande do Sul, Brazil
dDepartment of Internal Medicine, Medicine School of Federal University of Rio Grande do Sul (UFRGS), Porto Alegre, Rio Grande do Sul, Brazil
eRheumatology Department of the Porto Alegre University Hospital (HCPA), Porto Alegre, Rio Grande do Sul, Brazil
fCorresponding Author: Tiango Aguiar Ribeiro, Roraima Avenue nº 1000, University Campus, Santa Maria City, Rio Grande do Sul State, CEP 97105-900, Brazil
Manuscript accepted for publication February 08, 2016
Short title: Hospital Stay as a Protective Factor for Hip Fracture
doi: http://dx.doi.org/10.14740/jcs296e
| Abstract | ▴Top |
Background: Hip fracture is a devastating injury in elderly and the vast majorities are usually treated surgically. However, this treatment can also be non-operative, principally for patients classified at ASA III-IV. Several risk factors are associated with 1-year mortality for operated patients but a small number of studies provide the risk factors for non-operated patients. The aim of this study was to investigate the influence of hospitalization time and other risk factors on non-operated patients.
Methods: A prospective observational cohort study from April 2005 to April 2012 was conducted on 286 patients aged 65 years or more with hip fracture classified at ASA III-IV for 1 year to investigate the influence of hospitalization time and the 1-year mortality risk factors. Survival time was analyzed by Kaplan-Meier curves and Cox’s regression models were used to evaluate risk factors to all subjects, operated and non-operated subjects.
Results: The mortality was 73.5% for non-operated subjects. Final Cox’s regression for all subjects demonstrated that for patients that do not undergo surgery, mortality increased by six times. To operated patients, for each day of hospitalization, 1-year survival decreased 12.6 days, and ASA IV increased the mortality rate three times. To non-operated subjects, hospitalization time was a protective factor; for each day of hospitalization, 1-year survival increased 10.44 days.
Conclusion: When conservative treatment is chosen for a complicated elderly, extended hospitalization should be considered. Hospitalization time has proved to be a protective factor in these cases and discharge with improved survival rates with good clinical status should be advocated. However, surgery should always be employed even for patients with poor clinical conditions.
Keywords: Hip fracture; Elderly; Cohort study; One-year mortality risk factor; Length of hospitalization; Protective factor
| Introduction | ▴Top |
As the most common and devastating injury in the elderly, hip fractures [1] are associated with approximately 30% mortality in 1 year time [2, 3]. It is estimated that the number of these fractures may increase nearly 6.3 million in the next 40 years [4], and as a result of this catastrophic event, the elderly may develop a temporary or permanent impairment of independence and quality of life [2].
The treatment of hip fractures can offer some benefits, such as pain relief, early mobilization and reduced clinical complications. All of these benefits can improve the survival rate [5]. The treatment should take into account the fracture classification and may be conservative (nonsurgical) or surgical [6]. Hip fractures can be classified according to their anatomic localization: intracapsular fractures (femoral neck fractures) and extracapsular fractures (fractures in the trochanteric region). For undisplaced or impacted-undisplaced femoral neck fractures, some authors have suggested conservative treatment with acceptable outcomes [7-10], although other authors advocate surgery in all cases of femoral neck fractures (displaced and undisplaced) [11, 12]. For fractures of the transtrochanteric region, a review published in Cochrane [6] stated that there were no significant differences between surgical and non-surgical treatment. However, even with these two treatment options for these two different anatomical types of hip fracture, the vast majority of hip fractures are usually treated by surgical procedures [13], and some researchers have opined that conservative treatment should be chosen only for patients with severe comorbidities [13-15].
Several risk factors, such as male gender [13, 16-21], comorbidities [22], surgery delay [1, 13, 15], older age [13, 18, 23] and an elevated ASA score (American Society of Anesthesiologists physical status classification system) [19, 20, 23-25], are associated with 1-year mortality for operated patients, but few studies in the current literature [5, 13, 14, 26] describe the risk factors for non-operated patients.
Is the overall mortality rate in non-operated patients classified at ASA III-IV the same as that observed in operated patients classified at ASA III-IV? Is the mortality in non-operated patients the same as that observed and related in the current literature? Is there a difference in the survival time in any group? Do non-operated patients have the same risk factors for 1-year mortality as those already reported for surgical patients? Does the length of hospitalization have an important role in the 1-year mortality of non-operated patients compared to operated patients? In this study, we investigated the mortality rate and the risk factors associated with 1-year mortality in patients aged 65 years or more with a hip fracture classified at ASA III-IV treated by the conservative and the surgical methods in a tertiary public university hospital in south Brazil. The aim was to identify the real influence of hospitalization time on the 1-year mortality in these two distinct groups of hip fracture subjects.
| Methods | ▴Top |
A prospective observational cohort study was performed at the University Hospital of the Universidade Federal de Santa Maria (HUSM-UFSM) in southern Brazil after approval from the University Ethics Committee. The study followed the ethical guidelines of the 1975 Declaration of Helsinki. The inclusion time for subjects was from April 2005 to April 2012 and subjects were followed up for 1 year through regular medical appointments. All patients older than 65 years and diagnosed for hip fracture were eligible to be screened. Five hundred forty-four (544) patients were initially screened in these 8 years. According to inclusion and exclusion criteria, 286 patients were included in the final analysis.
Inclusion criteria were considered: the ASA at grade III to V.
Exclusion criteria were considered: patient refused to participate in this observational study by not signing the consent form.
The selected subjects were allocated into two groups: surgical group and non-surgical group. The choice of the conservative treatment (non-surgical) was not influenced by the research group as well as by this observational cohort study. The researchers just carried out the follow-up of these subjects. The choice of non-operative treatment was made by the surgical staff of our hospital based on at least one of two defined criteria: 1) patients classified in the ASA [27] grade III associated with the diagnosis of stroke and a bedridden condition; 2) patients classified at ASA [27] grade IV associated with bedridden condition.
On admission into hospital, information was collected regarding gender, age, fracture classification (neck, transtrochanteric or subtrochanteric), comorbidities (systemic arterial hypertension, ischemic heart disease, diabetes, stroke, asthma, chronic obstructive pulmonary disease and chronic renal failure), and discharge and in-hospital death date. Status surgery and ASA score were also collected. To the ASA score we considered: ASA III - patients with severe systemic diseases; ASA IV - patients with severe systemic diseases that were a constant threat to their life.
All subjects had an appointment scheduled 1 year after the fracture. All subjects who missed their appointment were contacted by telegram and by telephone call. Subjects who did not respond to the telegram or telephone call were considered to have missed the study.
Statistical analysis
The statistical analysis was conducted using SPSS version 18.0 (SPSS Inc., IBM Corporation, Armonk, NY). Quantitative variables were described as mean, standard deviation, median and interquartile range (IQR), and qualitative variables as frequencies. The ANOVA test was used to identify age and hospitalization time differences between groups. The survival time was analyzed by Kaplan-Meier curves and a log rank (Mantel-Cox) test was conducted to evaluate possible differences between groups regarding the survival time. The survival time was analyzed in three different ways, one with the whole study population, one with the operated subjects, and one with the non-operated subjects. Cox’s proportional hazard regression models were used to evaluate risk factors for 1-year mortality. The study population was analyzed in three different models to verify possible different mortality risk factors. One model used all subjects, one model used only operated subjects and one model used the non-operated subjects. In the univariate analysis, the variables with a P value < 0.05 were included in the multivariate analysis. The multivariate analysis was performed by the backward conditional method and final variables were considered significant in the multivariate analysis when the P value was < 0.05. The best model to assess the risk factors for mortality at 1 year was chosen considering the likelihood ratio. Differences in the study were considered to be significant when the P value was < 0.05.
| Results | ▴Top |
There was no loss of follow-up among the 286 patients included in this study. All subjects were analyzed. The mean age at the time of hospital admission was 81.7 ± 7.26 years (mean ± standard deviation), range 65 - 99 (82 (IQR 77 - 87)) (median (IQR)). Women were more prevalent (73.8%, n = 211) than men (26.2%, n = 75) in our study. Transtrochanteric fracture was the most common type of fracture with 60.8% (174), followed by femoral neck fracture with 36.7% (105) and subtrochanteric fracture with 2.4% (seven). The subjects’ ASA score distribution in our cohort was as follows: 82.2% (235) in ASA III and 17.8% (51) in ASA score IV. Seventy-one percent (203) of all subjects were treated surgically and 29% (83) were treated non-surgically. The general and specific groups subjects’ characteristics are displayed in Table 1. No age differences were observed in gender, fracture groups and ASA scores considering all subjects (P = 0.058, P = 0.176 and P = 0.105, respectively). In the operated group, we found significant age differences between genders and ASA score III-IV (P = 0.009 and P = 0.028, respectively); no age difference was found between fracture types (P = 0.119). In the non-operated group, no age differences were observed in gender, fracture groups and ASA scores (P = 0.624, P = 0.804 and P = 0.482, respectively).
 Click to view | Table 1. Population Characteristics |
Only 64.3% (184) patients were alive 1 year later (79.8% (162) in the operated group and 26.5% (22) in the non-operated group). The overall mortality was 35.7% (102) (20.2% (41) in the operated group and 73.5% (61) in the non-operated group). In-hospital mortality accounted for 58.82% (60) of all deaths (25% (15) in the operated group and 75% (45) in the non-operated group). Subjects who died were older than those who were alive in all study population (P < 0.001). Stratifying this result, we did not find differences in the surgical group (P = 0.071); however, we found differences in the non-surgical group (P = 0.003). The average age of survivors in non-operated group was 79 ± 8.7 years (79 (IQR 71 - 86)) compared to dead subjects 85 ± 6.7 years (85 (IQR 80 - 88)).
An interesting result was found concerning the hospitalization time between those who survived and those who died. In the general study population, the analysis was not statistically significant and no differences were encountered (P = 0.675). But in the operated group, the survival subjects had a less hospitalization time of 12 ± 8.6 days (10 (IQR 7 - 14)) compared to dead subjects 17 ± 12 days (14 (IQR 8 - 22)) (P = 0.004). In contrast from that observed in the non-operated group, the survivors had a longer hospitalization of 18 ± 17.2 days (13 (5 - 29)) versus 11 ± 10.8 days (8 (4 - 13)) when compared with those who died (P = 0.026). No differences were observed among different ASA scores in the hospitalization time for all subjects (P = 0.952), only for operated subjects (P = 0.585) and only for non-operated subjects (P = 0.975).
Kaplan-Meier curves demonstrated a 1-year overall survival for all subjects of the study of 263.88 ± 8.94 days (95% CI: 246.35 - 281.42), and a cumulated 1-year mortality risk of 44.18% (Fig. 1). Significant differences were observed in survival time by the log rank test in the surgical status (P < 0.001) and in the different ASA scores (P < 0.001) (Fig. 2). The survival analysis has shown an overall 1-year survival for operated subjects of 316.83 ± 7.66 days (95% CI: 301.82 - 331.83). The 1-year mortality risk was 22.62% (Fig. 1). The ASA scores had significant differences in 1-year survival in this group of patients (P = 0.002). For non-operated patients, the overall 1-year survival was 134.46 ± 17.64 days (95% CI: 99.89 - 169.03) and the overall 1-year mortality risk was 132.78% (Fig. 1). No differences were observed in the survival time between gender and ASA scores in this group.
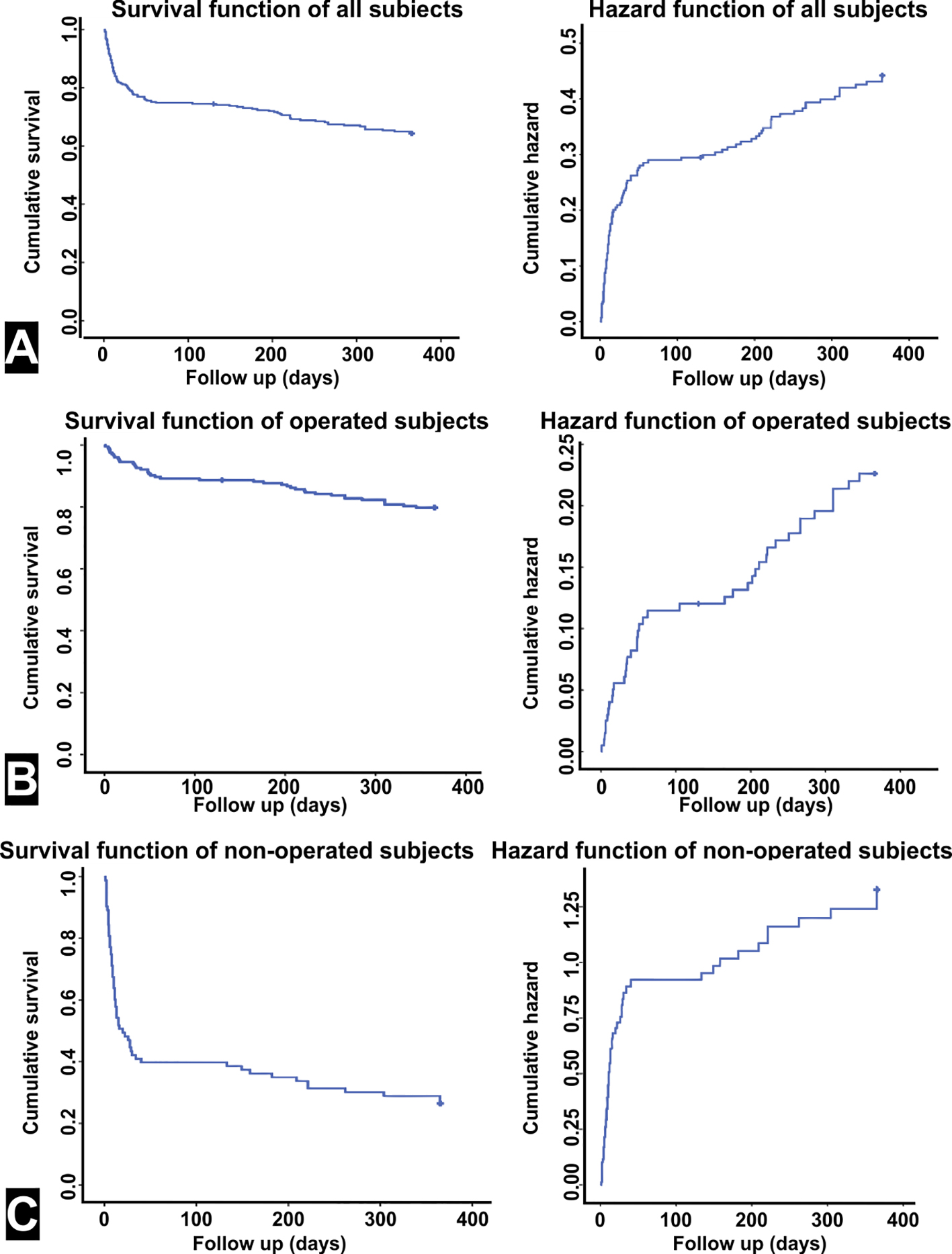 Click for large image | Figure 1. Survival time analyzed by Kaplan-Meier curves. (A) Analysis to all subjects. The survival time was 263.88 ± 8.94 days (64.28%) (left graph). The hazard cumulative risk to all subjects was 44.17% (right graph). (B) Analysis only for operated subjects. The survival time was 316.82 ± 7.66 days (79.75%) (left graph). The hazard cumulative risk to operated subjects was 22.62% (right graph). (C) Analysis only for non-operated subjects. The survival time was 134.45 ± 17.64 days (26.50%) (left graph). The hazard cumulative risk to non-operated subjects was 132.77% (right graph). |
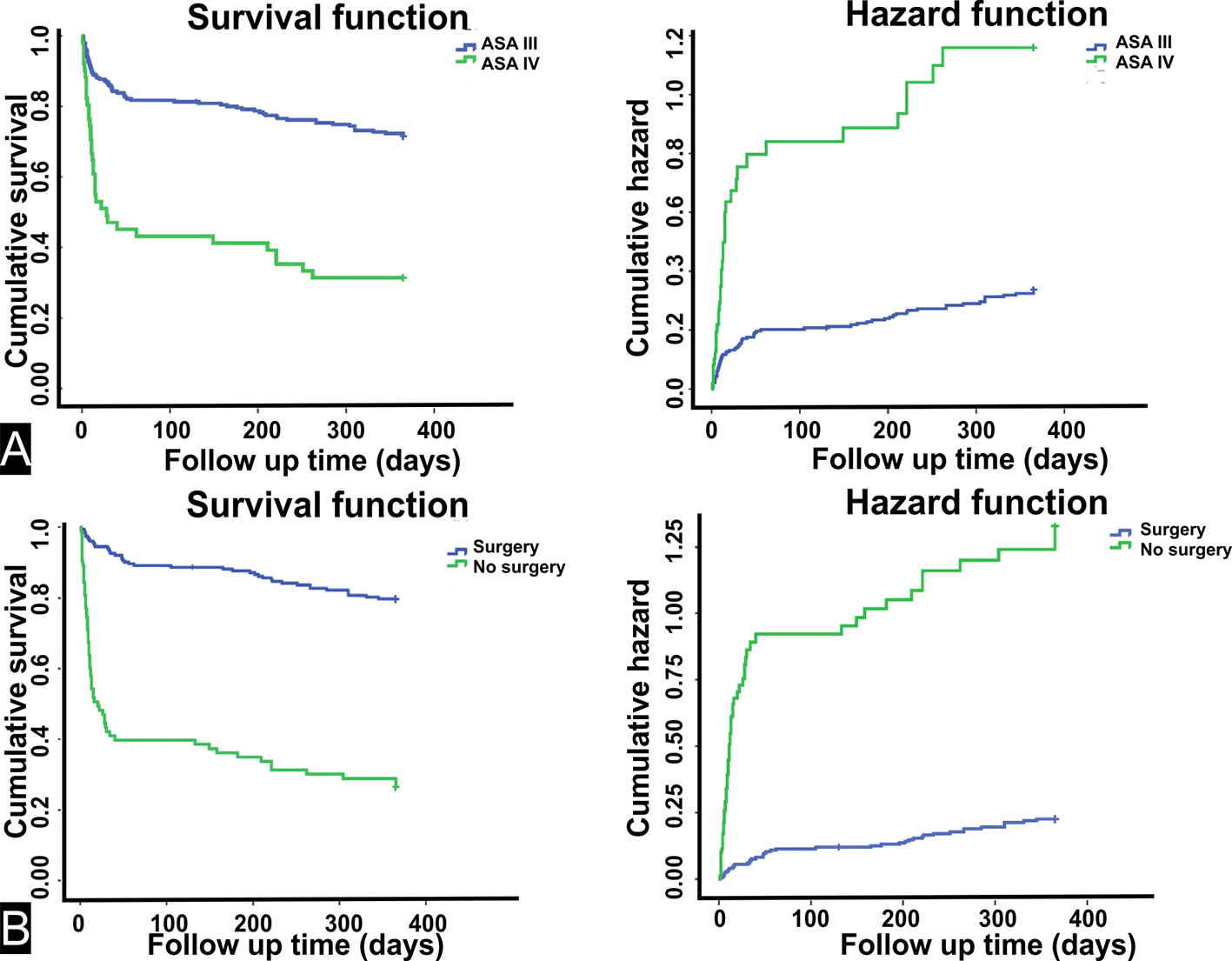 Click for large image | Figure 2. Comparison in the survival time for all subjects. (A) Comparing the survival time between ASA scores (ASA III and ASA IV), a difference was observed by the log rank test (Mantel-Cox) (P < 0.001). Left side: survival function graph. ASA III 289.09 ± 8.91 days (95% CI: 271.62 - 306.56) (71.44%) and ASA IV 147.78 ± 22.56 days (95% CI: 103.57 - 192) (31.37%). Right side: hazard function graph indicating the cumulative risk after 1 year (33.63% for ASA III and 115.92% for ASA IV). (B) Comparing the survival time between status surgery (surgery or no surgery), a difference was observed by the log rank test (Mantel-Cox) (P < 0.001). Left side: survival function graph. Surgery 316.83 ± 7.66 days (95% CI: 301.82 - 331.83) (79.75%) and no surgery 134.46 ± 17.64 days (95% CI: 99.89 - 169.03) (26.51%). Right side: hazard function graph indicating the cumulative risk after 1 year (22.62% for surgery and 132.78% for no surgery). |
One-year mortality predictors were analyzed by Cox regression models. In the univariate analysis for all subjects, age, ASA, status surgery and ischemic stroke were significant risk factors. These variables were analyzed in a multivariate analysis and the final model for 1-year risk factors for all subjects with hip fracture demonstrated that age and status surgery were significant (Table 2). For patients that did not undergo surgery, the mortality rate increased by six times. Table 3 demonstrates the univariate and multivariate analysis by taking into account only the group of operated patients. Age, ASA score and length of hospitalization were 1-year risk factors for mortality in this group. For each day of hospitalization, the 1-year survival decreased 12.6 days. An ASA score IV increased the mortality rate three times. To the non-operated group, the final Cox regression model demonstrated that only hospitalization time was significant, however, as a protective factor (Table 4). For each day of hospitalization, the 1-year survival increased 10.44 days. No risk factor for this group was found.
 Click to view | Table 2. One-Year Mortality Predictors to All Subjects |
 Click to view | Table 3. One-Year Mortality Predictors for Operated Subjects |
 Click to view | Table 4. One-Year Mortality Predictors for Non-Operated Subjects |
| Discussion | ▴Top |
Our overall mortality rate was higher, as well as our non-surgical group mortality rate. Hospitalization time proved to be a protective factor against 1-year mortality in non-operated group opposing to the operated group in which it has proved to be a risk factor. For each day of hospitalization, there was an increase of 10.44 days in the final 1-year survival of non-operated subjects. For each day of hospitalization, there was a decrease of 12.6 days in the final 1-year survival of operated patients. Within these two distinct groups (operated and non-operated), hospitalization time was different among death and survival subjects. Status surgery was considered a risk factor for all subjects and increased the mortality rate by six times if it was not performed.
Our mortality rate in non-operated patients was excessively high (73.5%) when compared to the mortality rate of operated patients (20.2%), as well as when compared to the already related mortality in operated patients (25.9-30%) [1, 18, 28]. Maybe the high mortality rate in our study can be attributed to the fact that these studies [1, 18, 28] used patients classified in all ASA scores and our study only use patients classified in ASA III and IV. This fact possibly decreased the overall mortality in these studies. But even higher our non-surgical mortality rate was similar to those presented by Gregory et al [5] (50%) and by Yoon et al [26] (64%) in the conservative treatment group of the studies. Most of the studies considering the mortality rate have shown the superiority of surgical treatment for hip fractures [29, 30]. However, a few authors have reported that there was no strong evidence [6] or no differences were observed in the mortality outcome between patients treated by the operative method and patients treated by the non-operative method [14]. Allied to these reports, some researchers have opined that conservative treatment should be chosen for patients with severe comorbidities [13-15]. But the fracture classification should be taken into account when considering the treatment for hip fractures in elderly subjects [6]. With regard to the anatomical classification of hip fractures, for femoral neck fractures, classified as undisplaced or impacted-undisplaced, the option for a conservative treatment may be an acceptable choice with reasonable outcomes [7-10]. For extra-capsular fractures, only one review discussed the two options of treatment [6], and the conclusion of the authors comparing conservative and surgical treatment was that no significant differences exist. But for extra-capsular hip fractures, the decision is very controversial. Conservative treatment implies prolonged bed rest and/or traction with associated complications, such as pressure sores, respiratory infection, urinary tract infection and thromboembolic events [14]. The limited scientific evidence about conservative treatment for extra-capsular fractures becomes this discussion irrelevant. In our study, the surgical staff opted for the non-surgical treatment for patients with severe comorbidities (ASA score of III in association with ischemic stroke and a bedridden condition or ASA score of IV associated with a bedridden condition). Because of this decision being made for the conservative treatment, the mortality rate was excessively high. For this reason, the opinion of our staff has changed with the results of this study and now follows the British Orthopaedic Association, which recommends surgical treatment for all hip fractures [31]. This is expected to offer some benefits to hip fracture patients such as pain relief, early mobilization, and reduced clinical and surgical complications, improving the survival rates [5].
In our study, we concluded that ASA score is a 1-year mortality risk factor only for operated subjects, as previously reported by several researchers [19, 20, 23-25]. In many publications in which subjects were treated surgically and were classified as having an ASA score of III or IV, the expected survival rate after 1 year is 79.75% [32], and we found a survival rate in these ASA scores of 81.63% (ASA III) and 50% (ASA IV). This proves that the clinical impairment has a crucial role when the operative treatment is chosen. To the non-surgical group, the ASA score was not a risk factor and hospitalization time was found as a protective factor. We conclude that the clinical status of patient in this group is not important, but the time that the patient remains hospitalized to improve it. Therefore, a hip fracture is an event that destabilizes elderly subjects with a high number of comorbidities [33], which deserves the attention of the medical staff in the management of these comorbidities in order to improve them.
The patients who died were older than those who were alive considering all the study population and in the non-operated population, and age was a risk factor for all subjects as observed in the model presented in Table 2. High rates of mortality were associated with older subjects and we believe that these patients require a longer hospitalization to improve their clinical status, since they did not undergo surgery. Frail elderly patients require not only orthopedic care but also care for their comorbidities [34], because hip fractures impair elderly people with many pathologies [33].
In this cohort, other characteristics such as type of fracture, gender and the presence or not of comorbidities were not found as risk factors for 1-year mortality as related in other studies in which only surgical treatment was chosen and all ASA scores were analyzed [13, 16, 18, 22, 23].
To date, we have found only two articles in the present literature that report the effect of length of hospitalization on the mortality rate of elderly patients who underwent surgery for a hip fracture [35, 36]. One of them reports that for every additional 10 days of hospitalization time, a significant reduction of 25.6% in the mortality risk was obtained [35]. Kondo et al in another article affirm that subjects who stayed for more than 40 days in hospital had a significantly lower risk than those who stayed 30 - 39 days [36]. However, other researchers [37, 38] have shown that prolonged hospitalization was a risk factor for fractured elderly subjects to develop complications. Reports on the increase of urinary tract infection associated with prolonged hospitalization time in patients who underwent surgery were made by Kamel [37]. Umarji et al [38] found that when the discharge takes more than 8 days, an increased number of hip fracture patients (58%) develop a nosocomial infection. Although these articles have certain divergent opinions, none of them, and no other paper, referred to the relationship between hospitalization time and mortality rate for non-operated patients. We believe that our study is the first to report this relation in elderly subjects with a hip fracture treated by the non-surgical method. A prolonged hospital stay serves to improve the clinical status of elderly patients and proved to be a protective factor in this select group of patients.
Our study has some limitations. The study design was not a randomized trial. Only patients with more severe clinical conditions such as bedridden and ischemic stroke condition were not operated by the surgical staff, which certainly increased the mortality rate of this select group. However, our study has several positive points including an appropriate statistical analysis and an adequate follow-up. Our sample was considerably very large and our cohort is one of the few that reported and discussed the 1-year mortality and 1-year risk factor of ASA III-IV hip fracture patients, as well as being the first to describe the protective relationship between length of hospitalization and 1-year mortality in non-operated elderly patients with a hip fracture.
Conclusion
When conservative treatment is chosen for a complicated elderly subject, an extended hospitalization for better clinical management should be considered. The hospitalization time has proved to be a protective factor in these cases and discharge with improved survival rates associated with good clinical status should be advocated. However, surgical treatment should always be employed even for patients with poor ASA scores, bedridden condition or ischemic stroke. The conservative treatment implies a prolonged period of rest, leading to the worsening of clinical status. The mortality rates are shown to be extremely high in these situations.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
| References | ▴Top |
- Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87(3):483-489.
doi pubmed - Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15(11):897-902.
doi pubmed - Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ. Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury. 2008;39(10):1157-1163.
doi pubmed - Sambrook P, Cooper C. Osteoporosis. Lancet. 2006;367(9527):2010-2018.
doi - Gregory JJ, Kostakopoulou K, Cool WP, Ford DJ. One-year outcome for elderly patients with displaced intracapsular fractures of the femoral neck managed non-operatively. Injury. 2010;41(12):1273-1276.
doi pubmed - Handoll HH, Parker MJ. Conservative versus operative treatment for hip fractures in adults. Cochrane Database Syst Rev. 20083):CD000337.
- Cserhati P, Kazar G, Manninger J, Fekete K, Frenyo S. Non-operative or operative treatment for undisplaced femoral neck fractures: a comparative study of 122 non-operative and 125 operatively treated cases. Injury. 1996;27(8):583-588.
doi - Raaymakers EL. The non-operative treatment of impacted femoral neck fractures. Injury. 2002;33(Suppl 3):C8-14.
doi - Folman Y, Gepstein R, Assaraf A, Liberty S. Functional recovery after operative treatment of femoral neck fractures in an institutionalized elderly population. Arch Phys Med Rehabil. 1994;75(4):454-456.
doi - Lyon LJ, Nevins MA. Management of hip fractures in nursing home patients: to treat or not to treat? J Am Geriatr Soc. 1984;32(5):391-395.
doi - Pearse EO, Redfern DJ, Sinha M, Edge AJ. Outcome following a second hip fracture. Injury. 2003;34(7):518-521.
doi - Shuqiang M, Kunzheng W, Zhichao T, Mingyu Z, Wei W. Outcome of non-operative management in Garden I femoral neck fractures. Injury. 2006;37(10):974-978.
doi pubmed - Shoda N, Yasunaga H, Horiguchi H, Matsuda S, Ohe K, Kadono Y, Tanaka S. Risk factors affecting inhospital mortality after hip fracture: retrospective analysis using the Japanese Diagnosis Procedure Combination Database. BMJ Open. 2012;2(3).
doi pubmed - Hossain M, Neelapala V, Andrew JG. Results of non-operative treatment following hip fracture compared to surgical intervention. Injury. 2009;40(4):418-421.
doi pubmed - Beringer TR, Crawford VL, Brown JG. Audit of surgical delay in relationship to outcome after proximal femoral fracture. Ulster Med J. 1996;65(1):32-38.
pubmed - Radcliff TA, et al. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Joint Surg Am. 2008;90(1):34-42.
doi pubmed - Aharonoff GB, Dennis MG, Elshinawy A, Zuckerman JD, Koval KJ. Circumstances of falls causing hip fractures in the elderly. Clin Orthop Relat Res. 1998;348:10-14.
doi pubmed - Tarazona-Santabalbina FJ, Belenguer-Varea A, Rovira-Daudi E, Salcedo-Mahiques E, Cuesta-Peredo D, Domenech-Pascual JR, Salvador-Perez MI, et al. Early interdisciplinary hospital intervention for elderly patients with hip fractures : functional outcome and mortality. Clinics (Sao Paulo). 2012;67(6):547-556.
doi - Endo Y, Aharonoff GB, Zuckerman JD, Egol KA, Koval KJ. Gender differences in patients with hip fracture: a greater risk of morbidity and mortality in men. J Orthop Trauma. 2005;19(1):29-35.
doi pubmed - Soderqvist A, Ekstrom W, Ponzer S, Pettersson H, Cederholm T, Dalen N, Hedstrom M, et al. Prediction of mortality in elderly patients with hip fractures: a two-year prospective study of 1,944 patients. Gerontology. 2009;55(5):496-504.
doi pubmed - Lin WP, Wen CJ, Jiang CC, Hou SM, Chen CY, Lin J. Risk factors for hip fracture sites and mortality in older adults. J Trauma. 2011;71(1):191-197.
doi pubmed - Arliani GG, et al. Correlacao entre tempo para tratamento cirurgico e mortalidade em pacientes idosos com fratura da extremidade proximal do femur. Revista Brasileira de Ortopedia. 2011;46(2):189-194.
doi - Guerra MTE, et al. Fratura do quadril: avaliacao pos operatoria do resultado clinico e funcional. Revista Brasileira de Ortopedia. 2010;45(6):577-582.
doi - Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77(10):1551-1556.
pubmed - Smektala R, Endres HG, Dasch B, Maier C, Trampisch HJ, Bonnaire F, Pientka L. The effect of time-to-surgery on outcome in elderly patients with proximal femoral fractures. BMC Musculoskelet Disord. 2008;9:171.
doi pubmed - Yoon BH, Baek JH, Kim MK, Lee YK, Ha YC, Koo KH. Poor prognosis in elderly patients who refused surgery because of economic burden and medical problem after hip fracture. J Korean Med Sci. 2013;28(9):1378-1381.
doi pubmed - Owens WD, Felts JA, Spitznagel EL, Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49(4):239-243.
doi pubmed - Elliott J, Beringer T, Kee F, Marsh D, Willis C, Stevenson M. Predicting survival after treatment for fracture of the proximal femur and the effect of delays to surgery. J Clin Epidemiol. 2003;56(8):788-795.
doi - Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M, McLaughlin M, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738-1743.
doi pubmed - Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87(8):1123-1126.
doi pubmed - The Care of Patients with Fragility Fracture. 2007. British Orthopaedic Association.
- Ribeiro TA, Premaor MO, Larangeira JA, Brito LG, Luft M, Guterres LW, Monticielo OA. Predictors of hip fracture mortality at a general hospital in South Brazil: an unacceptable surgical delay. Clinics (Sao Paulo). 2014;69(4):253-258.
doi - Boddaert J, Cohen-Bittan J, Khiami F, Le Manach Y, Raux M, Beinis JY, Verny M, et al. Postoperative admission to a dedicated geriatric unit decreases mortality in elderly patients with hip fracture. PLoS One. 2014;9(1):e83795.
doi pubmed - Wells JL, Seabrook JA, Stolee P, Borrie MJ, Knoefel F. State of the art in geriatric rehabilitation. Part I: review of frailty and comprehensive geriatric assessment. Arch Phys Med Rehabil. 2003;84(6):890-897.
doi - Kondo A, Zierler BK, Isokawa Y, Hagino H, Ito Y, Richerson M. Comparison of lengths of hospital stay after surgery and mortality in elderly hip fracture patients between Japan and the United States - the relationship between the lengths of hospital stay after surgery and mortality. Disabil Rehabil. 2010;32(10):826-835.
doi pubmed - Kondo A, Zierler BK, Hagino H. Relationship between the length of hospital stay after hip fracture surgery and ambulatory ability or mortality after discharge in Japan. Jpn J Nurs Sci. 2010;7(1):96-107.
doi pubmed - Kamel HK. The frequency and factors linked to a urinary tract infection coding in patients undergoing hip fracture surgery. J Am Med Dir Assoc. 2005;6(5):316-320.
doi pubmed - Umarji SI, Lankester BJ, Prothero D, Bannister GC. Recovery after hip fracture. Injury. 2006;37(8):712-717.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
