| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Case Report
Volume 6, Number 2, June 2016, pages 57-59
Dermatofibrosarcoma Protuberans: A Case Report and Review of Surgical Management
Shauna Trinha, b, c, Paul Hannaa, Kevin Petersena, Osama Elsawya
aDepartment of Surgery, St. Joseph’s Regional Medical Center, 703 Main Street, Paterson, NJ 07503, USA
bNew York Medical College, 40 Sunshine Cottage Rd, Valhalla, NY 10595, USA
cCorresponding Author: Shauna Trinh, Department of Surgery, St. Joseph’s Regional Medical Center, 703 Main Street, Paterson, NJ 07503, USA
Manuscript accepted for publication May 09, 2016
Short title: Dermatofibrosarcoma Protuberans
doi: http://dx.doi.org/10.14740/jcs302w
| Abstract | ▴Top |
Dermatofibrosarcoma protuberans (DFSP) is an uncommon cutaneous neoplasm with low to intermediate grade malignancy. While it rarely metastasizes, it is characterized by aggressive local infiltration and high recurrence. The etiology of DFSP remains unknown, but current research has shown that DFSP has specific histologic, immunohistochemical, and cytogenetic findings. We report a unique case of a 29-year-old female who presented with a dry, shallow ulcerated right posterior shoulder mass diagnosed as DFSP, and describe our surgical management.
Keywords: Dermatofibrosarcoma protuberans; COL1A1-PDGFB fusion gene; Soft tissue tumor
| Introduction | ▴Top |
Accounting for approximately 0.1% of all malignancies, dermatofibrosarcoma protuberans (DFSP) is an uncommon low to intermediate grade soft tissue tumor [1]. Its overall annual incidence is 4.1 cases per million persons with a higher incidence in women and blacks [2]. Additionally, the highest age-specific incidence is found to be between 35 to 44 years old [2]. While it is locally aggressive and highly recurrent, DFSP rarely metastasizes. Its 10-year relative survival rate is 99.1% [2]. Although the etiology of DFSP is unknown, it is associated with specific histologic, immunohistochemical, and cytogenetic findings that aid in its diagnosis. In this case report, we discuss a case of a 29-year-old female who presented with a dry, shallow ulcerated right posterior shoulder mass and review our surgical management.
| Case Report | ▴Top |
A 29-year-old female with no significant past medical history presented with a right posterior shoulder mass that recently became painful and ulcerated. The patient was unsure of how long the mass had been present but had become more aware of it over the past 2 - 3 months. She also reported recent skin changes over the mass, concerning for infection, but denied any erythema or discharge. The patient also denied any fevers or chills. The mass was indurated, mobile, tender, and approximately 2 × 2 cm in size. The mass also had a necrotic surface with a dry, shallow central ulcer measuring 1 × 0.7 cm (Fig. 1). Preoperative diagnosis was suspicious for an infected sebaceous cyst. A formal excision of the mass measuring 2.5 × 1.5 × 1.2 cm was performed, and pathology was significant for DFSP with positive margins. Hematology-oncology was consulted and recommended wide local re-excision with clear margins. No imaging was recommended. Seventy-six days after her first procedure, the patient underwent wide local re-excision of the right posterior shoulder mass. To allow for adequate surgical margins, a mass with 1 cm borders extending from the previous incision site was excised and sent for intraoperative frozen section evaluation. The mass measured 5.1 × 3.2 × 1.9 cm. Pathology showed lateral margins that were negative for neoplastic cells but the deep segment demonstrated focal spindle cell proliferation uncertain for DFSP or reactive fibroblastic scar. The intraoperative diagnosis was indeterminate at that time, and the decision to continue with wound closure was made. Immunohistochemical staining completed 4 days after the procedure confirmed focal spindle cell proliferation favoring reactive fibroblastic scar. Because the margins were negative, postoperative radiotherapy was not recommended, and the patient will be followed up on an as needed basis.
 Click for large image | Figure 1. Gross image presents an indurated, mobile, tender mass with a central ulcer. |
| Discussion | ▴Top |
DFSP is an uncommon slow growing soft tissue tumor of low to intermediate grade malignancy. It is a locally aggressive cutaneous neoplasm with a high recurrence rate, but metastasis is rare. Histologically, DFSP is characterized by spindle cell proliferation. Spindle cells present in the dermal layer are arranged in a uniform storiform pattern. The neoplastic cells have little pleomorphism, no atypia, and a low mitotic index [3, 4]. In addition, the tumor often infiltrates underlying subcutaneous and muscle tissue, resulting in a honeycomb appearance. Immunohistochemistry is another useful tool for diagnosis of DFSP. On immunohistochemical stain, DFSP is typically positive for the CD34 marker. Furthermore, cytogenetic findings have shown that over 90% of DFSP tumors express either a reciprocal t(17;22)(q22;q13) translocation or supernumerary ring chromosomes derived from t(17;22) [2, 4]. This chromosomal rearrangement causes the fusion of the collagen type 1-alpha 1 (COL1A1) and platelet-derived growth factor beta (PDGFB) genes. The resulting COL1A1-PDGFB fusion gene promotes fibroblastic cell growth by upregulating the PDGFB receptor pathway [5].
Histopathology of our patient’s right posterior shoulder mass from her first excision procedure revealed spindle cells in a storiform pattern characteristic of DFSP (Fig. 2). Subsequent immunohistochemical stain was CD34+, verifying the diagnosis of DFSP (Fig. 3). Because of positive margins, the patient underwent a wide local re-excision, and histopathology showed focal spindle cell proliferation indeterminate for DFSP or reactive fibroblastic scar. An immunohistochemical stain followed and showed no positive CD34 markers in the areas of interest, thus favoring the diagnosis of reactive fibroblastic scar. Histology and immunohistochemistry are the gold standard in diagnosing DFSP. While fluorescence in situ hybridization (FISH) may be used to identify the COL1A1-PDGFB fusion gene, it is neither necessary nor definitive for diagnosis [6].
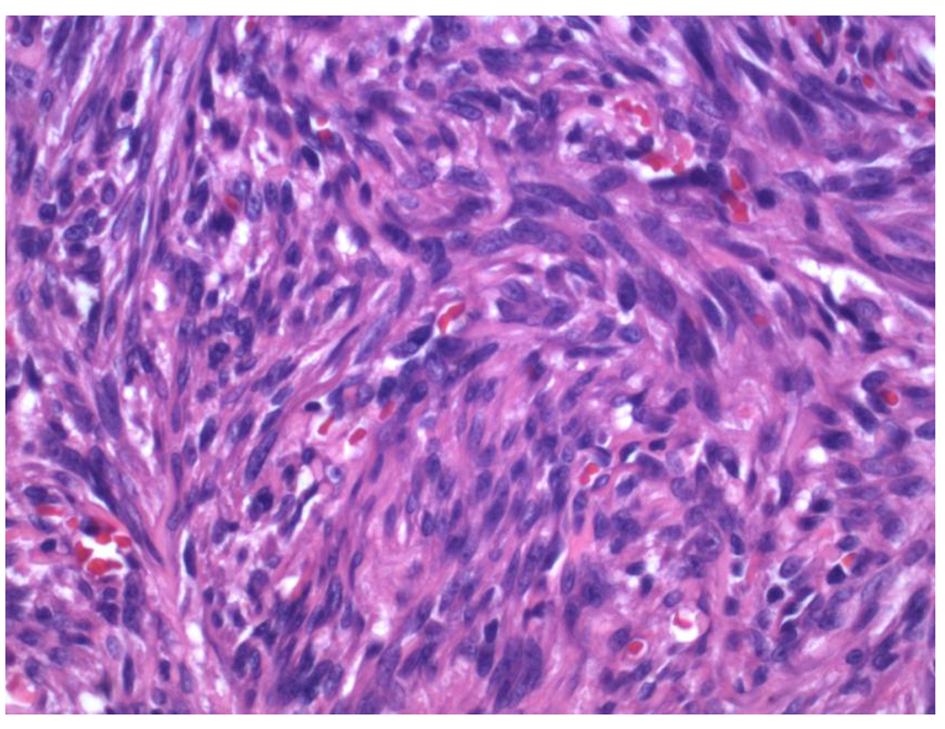 Click for large image | Figure 2. H&E stain demonstrates spindle cells arranged in a uniform storiform pattern. |
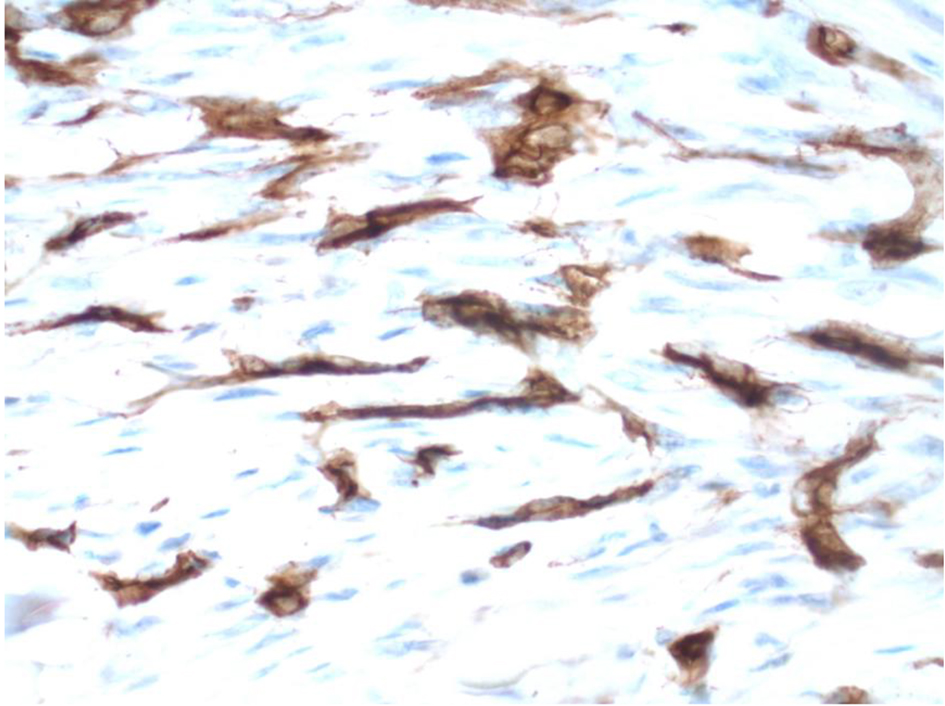 Click for large image | Figure 3. Immunohistochemical stain reveals CD34+ markers. |
The standard of treatment for localized DFSP is surgical resection. Wide local excision is the therapeutic choice, but Mohs micrographic surgery (MMS) has recently shown favored outcomes. While MMS can be more labor intensive and time consuming, it is associated with lower recurrence rates and superior cosmetic results [7]. In addition, because of DFSP’s unique cytogenetic findings, advancements have been made in medical treatment for locally advanced and metastatic DFSP. Imatinib mesylate is a tyrosine kinase inhibitor, which can be used to target PDGFB receptor and block PDGFB signaling [4].
Conclusion
DFSP is a rare cutaneous tumor characterized by aggressive local spindle cell proliferation, high recurrence, and a low metastatic potential. It can be identified by its specific histologic, immunohistochemical, and cytogenetic findings. While the mainstay of management in local disease is surgical excision, in locally advanced and unresectable metastatic disease, treatment has been limited to imatinib mesylate. Further investigation into the etiology and biology of DFSP is crucial for identifying novel markers and advancing current treatment.
| References | ▴Top |
- Criscione VD, Weinstock MA. Descriptive epidemiology of dermatofibrosarcoma protuberans in the United States, 1973 to 2002. J Am Acad Dermatol. 2007;56(6):968-973.
doi pubmed - Kreicher KL, Kurlander DE, Gittleman HR, Barnholtz-Sloan JS, Bordeaux JS. Incidence and Survival of Primary Dermatofibrosarcoma Protuberans in the United States. Dermatol Surg. 2016;42(Suppl 1):S24-31.
doi pubmed - Zheng Z, Piao J, Lee JH, Kim SE, Kim SC, Chung KY, Roh MR. Dermatofibrosarcoma protuberans: a study of clinical, pathologic, genetic, and therapeutic features in Korean patients. Yonsei Med J. 2015;56(2):440-446.
doi pubmed - Noujaim J, Thway K, Fisher C, Jones RL. Dermatofibrosarcoma protuberans: from translocation to targeted therapy. Cancer Biol Med. 2015;12(4):375-384.
pubmed - Simon MP, Navarro M, Roux D, Pouyssegur J. Structural and functional analysis of a chimeric protein COL1A1-PDGFB generated by the translocation t(17;22)(q22;q13.1) in Dermatofibrosarcoma protuberans (DP). Oncogene. 2001;20(23):2965-2975.
doi pubmed - Karanian M, Perot G, Coindre JM, Chibon F, Pedeutour F, Neuville A. Fluorescence in situ hybridization analysis is a helpful test for the diagnosis of dermatofibrosarcoma protuberans. Mod Pathol. 2015;28(2):230-237.
doi pubmed - Paradisi A, Abeni D, Rusciani A, Cigna E, Wolter M, Scuderi N, Rusciani L, et al. Dermatofibrosarcoma protuberans: wide local excision vs. Mohs micrographic surgery. Cancer Treat Rev. 2008;34(8):728-736.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
