| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website https://www.currentsurgery.org |
Case Report
Volume 11, Number 2, June 2021, pages 35-38
A Case of Intracholecystic Papillary-Tubular Neoplasm
Muhammad Darwisha, Houssam Osmana, Edward Choa, b, Wareef Kabbanic, Terence Jacksona, Kei Nagatomoa, D. Rohan Jeyarajaha, b, d
aDepartment of Surgery, Methodist Richardson Medical Center, 2805 East President George Bush Highway, Richardson, TX 75082, USA
bDepartment of Surgery, TCU/UNTHSC School of Medicine, Fort Worth, TX, USA
cDepartment of Pathology, Methodist Health System, Dallas, TX, USA
dCorresponding Author: D. Rohan Jeyarajah, Department of Surgery, Methodist Richardson Medical Center, 2805 East President George Bush Highway, Richardson, TX 75082, USA
Manuscript submitted April 9, 2021, accepted April 20, 2021, published online June 28, 2021
Short title: A Case of ICPN
doi: https://doi.org/10.14740/jcs408
| Abstract | ▴Top |
The World Health Organization (WHO) defines intracholecystic papillary neoplasms (ICPNs) as gallbladder lesions of intraductal papillary neoplasms of the bile duct (IPNB). We present a case of ICPN that was incidentally diagnosed following a cholecystectomy for cholecystitis and cholelithiasis. Abdominal ultrasonography and computed tomography showed thickening of the gallbladder wall and cholelithiasis but were not specific for a gallbladder tumor. Histopathological examination revealed an intracholecystic papillary-tubular neoplasm associated with a moderately differentiated adenocarcinoma.
Keywords: Intracholecystic papillary-tubular neoplasm; ICPN; Cholecystitis; Cholelithiasis cholecystectomy
| Introduction | ▴Top |
Intracystic papillary neoplasm is a form of intraluminal papillary neoplasms of the extrahepatic biliary tree that occurs in the gallbladder. The World Health Organization (WHO) defines intracholecystic papillary neoplasms (ICPNs) as gallbladder lesions of intraductal papillary neoplasm of the bile duct. ICPN is a preinvasive lesion that can have a pancreatobiliary or intestinal phenotype and may be associated with invasive adenocarcinoma which should be staged separately [1]. Here we discuss a case that presented with symptoms of acute cholecystitis and a ventral incisional hernia, and was incidentally found to have an ICPN associated with an intramucosal adenocarcinoma.
| Case Report | ▴Top |
Investigations
This patient is a 64-year-old male admitted to the hospital with right upper quadrant pain associated with nausea and vomiting. The patient had a past history of a ventral incisional hernia that was repaired with an underlay biologic mesh 6 years prior to presentation. He had undergone distal pancreatectomy and splenectomy for a pancreatic neuroendocrine tumor 8 years prior to presentation. Blood tests on admission showed white blood cell (WBC) 8.7 (normal range: 3.8 - 10.6 × 103/µL), red blood cell (RBC) 3.03 (normal range: 4.5 - 5.9 × 106/µL), hemoglobin (Hb) 7.8 (normal range: 13.5 - 17.5 g/dL), hematocrit (HCT) 25.6% (normal range: 40.2-50.2%), mean corpuscular volume (MCV) 84.5 (normal range: 80 - 100 fL), mean corpuscular hemoglobin (MCH) 25.7 (normal range: 26 - 34 pg), mean corpuscular hemoglobin concentration (MCHC) 30.5 (normal range: 31.1 - 36.6 g/dL), blood cell distribution width (RDW)-coefficient of variation (CV) 15.4 (normal range: 11.5-14.5%), platelets 155 (normal range: 130 - 400 × 103/µL). Abdominal computed tomography (CT) scan showed recurrent ventral hernia and cholelithiasis with no other acute findings (Fig. 1). Abdominal ultrasonography showed cholelithiasis with thickening of the gallbladder wall (Fig. 2). A hepato-iminodiacetic acid (HIDA) scan revealed non-visualization of the gallbladder consistent with cholecystitis.
 Click for large image | Figure 1. Abdominal computed tomography showing cholelithiasis (two black arrowheads). |
 Click for large image | Figure 2. Abdominal ultrasound showing cholelithiasis (white arrowhead). |
Diagnosis and treatment
A diagnosis of acute cholecystitis and cholelithiasis was made and the patient was scheduled for surgery. He underwent open cholecystectomy due to prior extensive surgeries and the need to repair the ventral hernia. Resection and anastomosis of a segment of small bowel was performed due to extensive adhesions. The gallbladder was distended with surrounding adhesions consistent with the diagnosis of chronic cholecystitis. The macroscopic findings of the resected specimen showed an intact saccular gallbladder measuring 14.0 × 7.5 × 6.0 cm in size with a lilac serosa. The gallbladder wall measured 0.2 cm and the mucosa was bile stained velvety with yellow stippling. There was a 4.5 × 2.5 × 0.8 cm exophytic soft mass, 1.0 cm from the cystic duct margin. The lumen contained a green thick sludge and yellow calculi measuring 3.5 × 3.0 × 2.0 cm in aggregate. Microscopic findings showed an intracholecystic papillary-tubular neoplasm (Figs. 3, 4) involving the lamina propria associated with a moderately differentiated biliary type intramucosal adenocarcinoma (Fig. 5). Cholelithiasis and cholesterolosis were present. The ICPN does not invade into the muscularis and had no lymphovascular or perineural invasion. The cystic duct margin was uninvolved, and no lymph nodes were dissected. Pathology stage was pT1aNXM0.
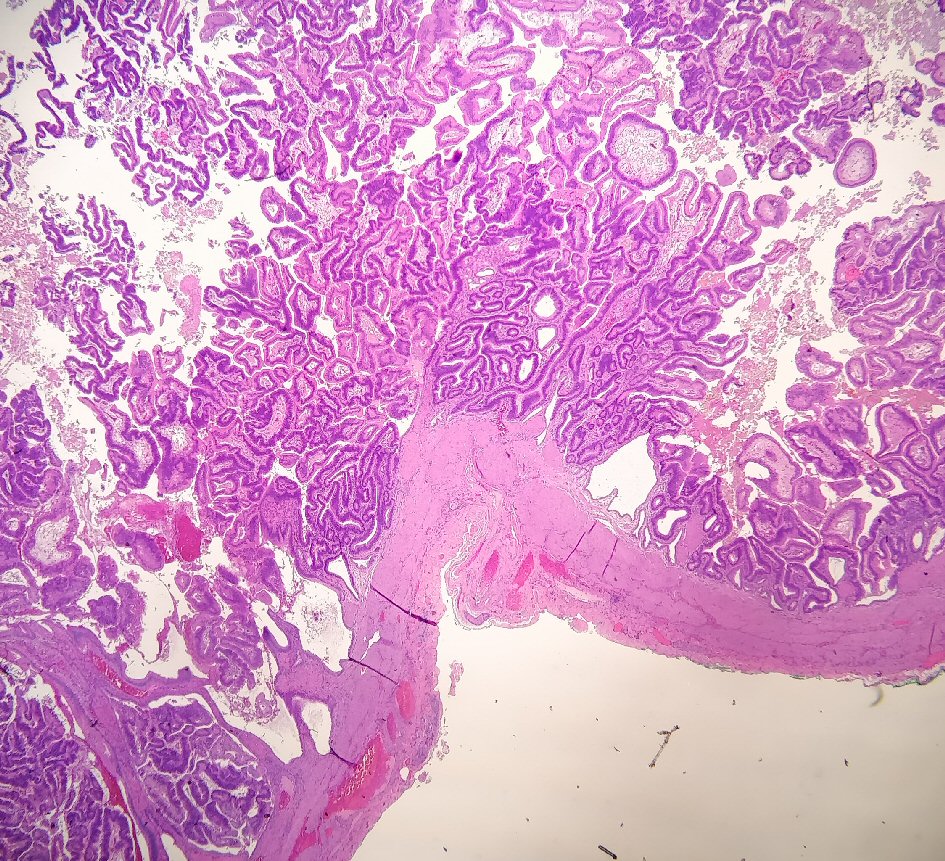 Click for large image | Figure 3. Histology slide (× 100) showing intracholecystic papillary-tubular neoplasm involving the lamina propria. |
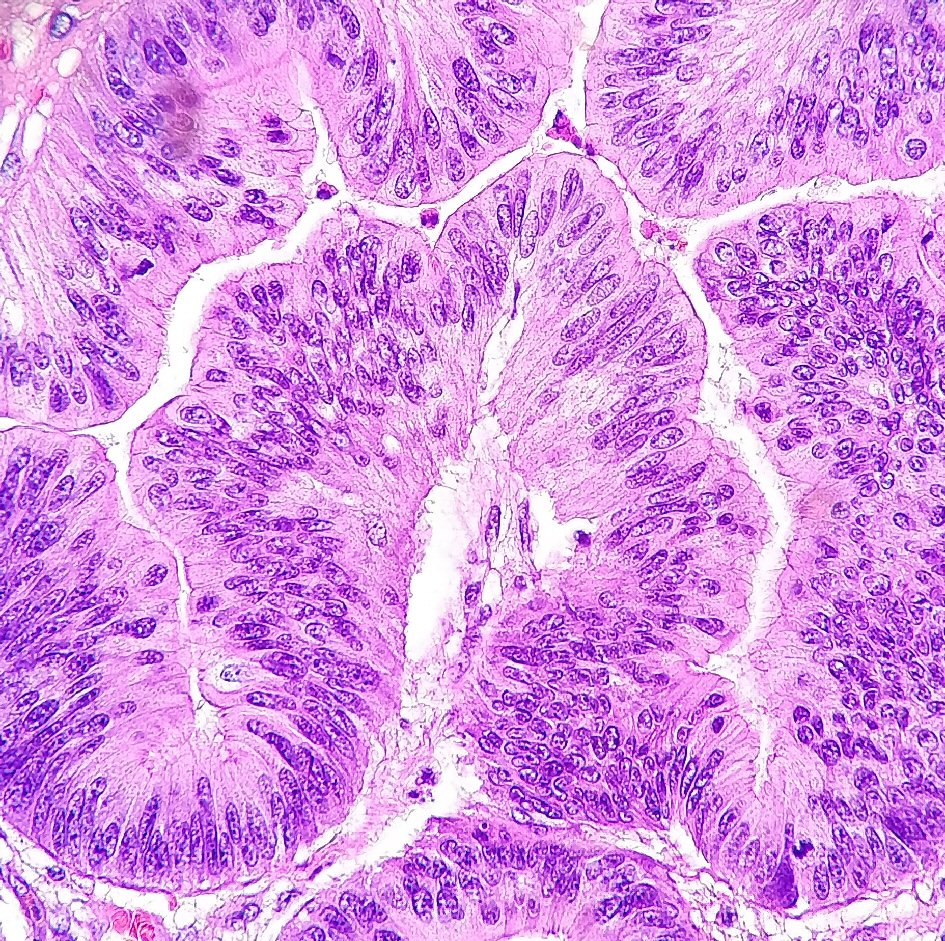 Click for large image | Figure 4. Histology slide (× 400) showing intracholecystic papillary-tubular neoplasm involving the lamina propria. |
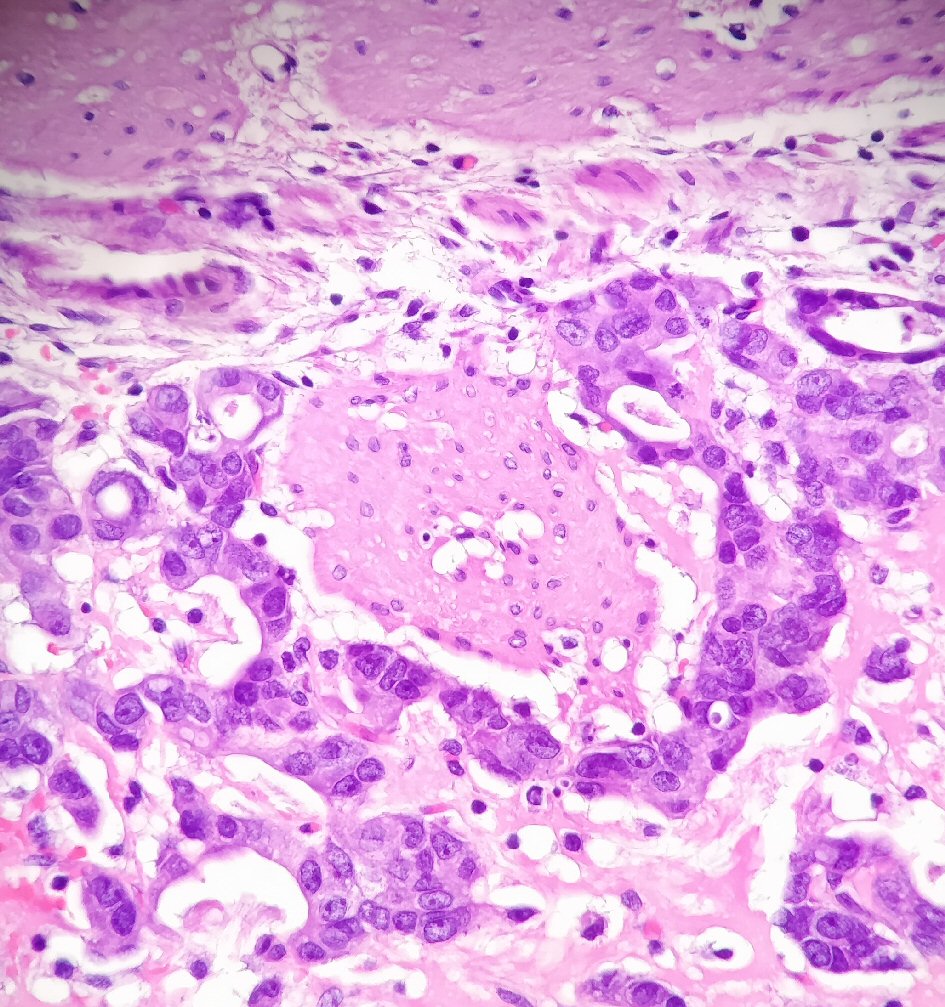 Click for large image | Figure 5. Histology slide (× 400) showing a moderately differentiated biliary type intramucosal adenocarcinoma. |
Outcome and follow-up
The post-operative period was complicated by respiratory failure, but the patient made a full recovery and was discharged home. The patient was seen 3 months after the surgery in the clinic and was completely asymptomatic and doing well.
| Discussion | ▴Top |
This case is presented as a rare diagnosis of ICPN presenting as an incidental finding in the gallbladder. The lack of specific symptoms and the incidental nature of the diagnosis are unfortunately common in ICPN cases. This case illustrates such diagnostic challenge which can lead to a later diagnosis at a more advanced stage. On the other hand, patients diagnosed early and treated with prompt surgical removal have excellent prognosis as was observed in this patient. The rarity of ICPN and the difficulties associated with detecting it are reflected by the limited number of reported cases and studies on it with the largest study entirely involving 123 cases. This can further be appreciated in its diagnostic criteria that have remained relatively ambiguous until rather recently. Given that, the aim of this report is to expand on the existing literature and to contribute to the modest volume of reported ICPN cases.
The American Cancer Society estimates that 11,980 adults in the USA will be diagnosed with gallbladder and other biliary cancers in 2020 resulting in around 4,090 deaths. Around 40% of said cases are specifically gallbladder cancers. The overall 5-year survival rate of gallbladder cancer is 19% but can vary depending on the staging and time of diagnosis. Localized and metastasized gallbladder carcinomas have a 5-year survival rate of 62% and 2% respectively [2]. On the other hand, the rarer ICPN with an incidence rate of < 0.5-0.61% tends to have a relatively indolent course and a significantly better prognosis with a 5-year survival rate of 78% and 60% in its non-invasive and invasive forms respectively [3, 4]. ICPN appears to evolve into invasive carcinoma in around 6.4% of cases which accounts for a tiny fraction of invasive carcinoma of the gallbladder considering the rare overall incidence of ICPN [3].
While gallbladder cancer usually affects patients in their sixth or seventh decade of life with a higher incidence in females, ICPN appears to affect a wider yet slightly younger age range with a mean age of 61 years, and has a 2.1:1 female/male ratio [1, 3]. Gallstones are considered a contributing risk factor for gallbladder cancer with more than 80% of carcinoma cases presenting with gallstones even though less than 0.2% of patients with cholelithiasis develop carcinoma of the gallbladder [1]. It is estimated that 20% of all ICPN cases present with associated cholelithiasis [3].
Around half of all ICPN and gallbladder carcinomas are diagnosed incidentally with other half usually presenting with non-specific symptoms such as right upper quadrant pain resembling chronic cholecystitis [1, 3]. Imaging studies such as CT and ultrasonography may aid in the detection of gallbladder neoplasms [1]. This patient’s abdominal ultrasound and CT showed cholelithiasis and gallbladder wall thickening but was not particularly specific for a mass. Imaging may not be able to distinguish between a gallbladder stone and a tumor which highlights the difficulty of detecting ICPNs radio-graphically as has been shown in other studies. Some studies estimate that up to half of ICPN cases are detected incidentally and up to 10% are missed on imaging studies [3].
The 2010 WHO classification introduced the definition of intracystic papillary neoplasm as gallbladder lesions of intraductal papillary neoplasm of the bile duct (IPNB). Intracystic papillary neoplasm is classified as a premalignant lesion of the biliary system. The classification does not provide specific diagnostic criteria but rather classifies intracystic papillary neoplasm into intraluminal papillary neoplasms as opposed to adenomas [1]. These two categories were unified to form “intracholecystic papillary neoplasms” in 2012 by Adsay et al [3]. In their study, Adsay et al defined ICPNs as gallbladder neoplasms that are intramucosal, preinvasive neoplastic (dysplastic), mass forming and exophytic, compact, ≥ 1.0 cm in size, and distinct from the neighboring mucosa [3].
ICPN is a form of intraluminal papillary neoplasms of the extrahepatic biliary tree that occurs in the gallbladder. Low-grade lesions were previously referred to as “papillary adenomas” whereas high-grade lesions were referred to as “non-invasive papillary carcinomas”. Invasive adenocarcinoma may arise with intracystic papillary neoplasms. Such lesions usually have high-grade intraepithelial neoplasia characterized by complex papillary structures and should be reported and staged separately [1].
ICPN and IPNB are histologically similar [1]. IPNB shares features with intraductal papillary mucinous neoplasm (IPMN) of the pancreas including intraluminal growth [5]. The main difference between ICPN and IPNB is the anatomical location of the neoplasm. Other key distinguishing features include greater architectural complexity, cytological atypia, and increased mitotic figures seen in high-grade intracystic papillary neoplasms. The majority of ICPNs have a biliary phenotype as opposed to the intestinal phenotype of papillary adenomas but they may overlap and can be difficult to distinguish from each other [1].
Prognosis for patients presenting with gallbladder cancer generally depends on the histological type and extent of the disease. Adenocarcinomas of the gallbladder confined to the lamina propria appear to be cured with a simple cholecystectomy as they do not metastasize. However, invasive adenocarcinomas extending through the entire thickness of the gallbladder wall have a 10-year survival rate of 30%. The best prognosis is associated with non-invasive intracystic papillary neoplasms as they rarely metastasize regardless of size, cell phenotype, and degree of differentiation with a 5-year survival rate of 78% [1, 3]. This patient had an early stage lesion and should be cured with a simple cholecystectomy. He was felt to not require further surgery due to the early T-stage.
Conclusions
ICPN is an uncommon tumor of the gallbladder that can be challenging to identify and diagnose both clinically and radio-graphically especially when accompanied by a different pathological process. This case report demonstrates the diagnostic challenge in a case presenting with acute symptoms obscuring an underlying ICPN.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Subject consent has been waived under the IRB-approved study protocol and the identity of the subject has been protected.
Author Contributions
Each named author has substantially contributed to conducting the underlying research and drafting this manuscript.
Data Availability
Data supporting the findings of this study are available within the article.
| References | ▴Top |
- Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system (No. Ed. 4). World Health Organization. 2010:11. Book Chapter.
- Cancer.org. 2020. Key statistics for gallbladder cancer. [online] Available at: https://www.cancer.org/cancer/gallbladder-cancer/about/key-statistics.html.
- Adsay V, Jang KT, Roa JC, Dursun N, Ohike N, Bagci P, Basturk O, et al. Intracholecystic papillary-tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are >/=1.0 cm): clinicopathologic and immunohistochemical analysis of 123 cases. Am J Surg Pathol. 2012;36(9):1279-1301.
doi pubmed - Argon A, Barbet FY, Nart D. The relationship between intracholecystic papillary-tubular neoplasms and invasive carcinoma of the gallbladder. Int J Surg Pathol. 2016;24(6):504-511.
doi pubmed - Bennett S, Marginean EC, Paquin-Gobeil M, Wasserman J, Weaver J, Mimeault R, Balaa FK, et al. Clinical and pathological features of intraductal papillary neoplasm of the biliary tract and gallbladder. HPB (Oxford). 2015;17(9):811-818.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
