| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Case Report
Volume 4, Number 1, February 2014, pages 31-33
Acute Emphasematous Cholecystitis
Radwan Kassira, c, Gabriella Ferraria, Claire Boutetb, Jack Porcherona
aDepartment of Digestive Surgery, CHU Hospital, Jean Monnet University, Saint Etienne, France
bDepartment of Radiology, CHU Hospital, Jean Monnet University, Saint Etienne, France
cCorresponding author: Radwan Kassir, Department of Digestive Surgery, CHU Hospital, Jean Monnet University, Avenue Albert Raimond, 42270 Saint Etienne, France
Manuscript accepted for publication December 20, 2013
Short title: Acute Emphasematous Cholecystitis
doi: https://doi.org/10.14740/jcs216w
| Abstract | ▴Top |
Emphysematous cholecystitis (EC) is an uncommon variant of acute cholecystitis and can be rapidly lethal. We report an extremely rare case of EC and we present the imaging features of this patient. An 80-year-old male presented with epigastric pain and fever. Abdominal computed tomography confirmed the presence of an air-liquid level in the gallbladder lumen, gas within the gallbladder and in its walls. Emergency open cholecystectomy revealed necrotic changes in the gallbladder. The patient’s postoperative course was uneventful. The mortality associated with non-emphysematous is 4% compared with 15% for EC due to the increased incidence of gallbladder wall gangrene and perforation. The pathophysiology of EC differs from that in acute calculous cholecystitis. Diagnosis is established when the CT scan reveals gas within the gallbladder or in its walls in the absence of an abnormal communication between the gastrointestinal tract and the biliary system. The standard treatment is emergent cholecystectomy and antibiotic therapy. It could conclude that surgeons should be aware of the existence of this kind of atypical presentation of cholecystitis. EC is a rare condition in which the abdominal computed tomograph proves to be a most useful tool. It is important to differentiate this rare pathologic feature of the gall bladder from other cholecystitis as the treatment is surgical rather than medical.
Keywords: Gall bladder; Cholecystitis; Emphysematous; CT scan; Surgery; Management
| Introduction | ▴Top |
Emphysematous cholecystitis (EC) is an uncommon variant of acute cholecystitis and can be rapidly lethal. EC is characterized by the presence of intramural and/or intraluminal gas and is a consequence of a primary ischemic injury. An early diagnosis and treatment are required.
| Case Report | ▴Top |
We report an extremely rare case of EC and we present the imaging features of this patient. An 80-year-old male presented with epigastric pain and fever. He had a history of diabetes mellitus. He presented with vomiting and acute abdominal syndrome. Clinical examination and laboratory assessment suggested acute cholecystitis.Abdominal computed tomography confirmed the presence of an air-liquid level in the gallbladder lumen, gas within the gallbladder and in its walls (Fig. 1, 2). The CT scan revealed no biliary obstruction or bile duct stones.Emergency open cholecystectomy revealed necrotic changes in the gallbladder. No gallstones were detected in the gallbladder. Antibiotic treatment was given pre and post-operation. The patient’s postoperative course was uneventful.
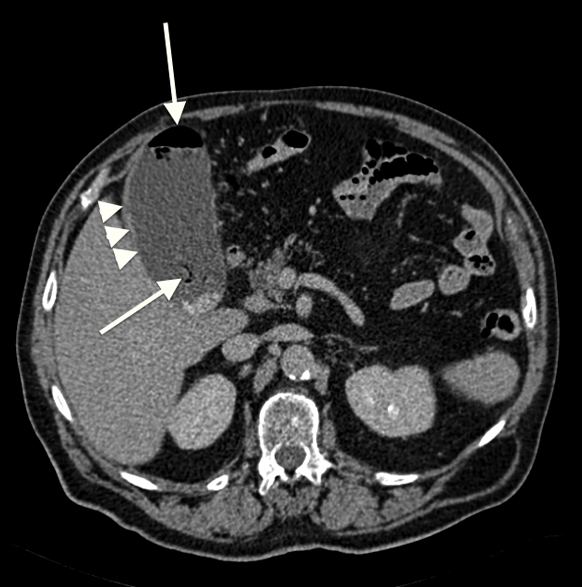 Click for large image | Figure 1. CT scan (axial axis) shows air in the gall bladder lumen with an air-fluid level (arrow) and gall bladder wall thickening (arrowhead). |
 Click for large image | Figure 2. CT scan (sagittal axis) shows air in the gall bladder lumen (arrow) with intramural air (arrowhead) without cholelithiasis or intrahepatic abscess. |
| Discussion | ▴Top |
EC is first described by May and Strong in 1971 [1]. EC is a rare variant and a life-threatening form of acute cholecystitis caused by ischemia of the gallbladder wall. CE is more common in patients with diabetes mellitus [2] and is an uncommon occurrence in the children [3]. The mortality associated with non-emphysematous is 4% compared with 15% for EC due to the increased incidence of gallbladder wall gangrene and perforation [2].
The pathophysiology of EC differs from that in acute calculous cholecystitis. The ischemia of the gallbladder wall allows mural translocation of gas-forming bacteria. Causative organisms previously reported include Clostridium perfringens, Clostridium welchii, Klebsielles, E. coli, and anaerobic Streptococci [4]. The bacteria most frequently cultured are Clostridia then Escherichia coli.
For identification of air within the biliary tract, several imagings can be used: plain radiography, ultrasound and CT. Ultrasonography demonstrates a characteristic “effervescent gallbladder”. CT scan is the most sensitive and specific [5]. Diagnosis is established when the CT scan reveals gas within the gallbladder or in its walls in the absence of an abnormal communication between the gastrointestinal tract and the biliary system. Miyahara et al described a case of EC with massive gas in the abdominal cavity. In our case, the CT scan does not reveal gas within the abdominal cavity [6].
EC is associated with a higher incidence of complications in comparison with acute cholecystitis [7]. Delgado-Plasencia et al concluded that should be considered as a possible cause of pneumomediastinum [8]. EC should be considered as a possible cause of soft tissue gas gangrene [9]. Simultaneous occurrence of EC and emphysematous pancreatitis is an exceptional and potentially fatal combination [10].
The base of treatment of this disease includes: cholecystectomy, drainage, appropriate antibiotic treatment and hyperbaric oxygenation [11]. The standard treatment is emergent cholecystectomy and antibiotic therapy. EC can be safely treated by the laparoscopic approach [4]. In our case, we realized open cholecystectomy. In severely ill patients, the standard treatment is emergent percutaneous cholecystostomy with broad-spectrum antibiotics [12]. Percutaneous cholecystostomy should be considered as a possible cause of musculoskeletal complications [13].
Conclusion
EC should be considered as a possible cause of acute abdominal syndrome, especially in diabetic patients. Prompt abdominal imaging is essential in making the correct diagnosis. EC requires aggressive medical and surgical treatment. Surgeons should be aware of the existence of this kind of atypical presentation of cholecystitis.
Conflict of Interest Statement
No.
| References | ▴Top |
- May RE, Strong R. Acute emphysematous cholecystitis. Br J Surg. 1971;58(6):453-458.
doi - Moanna A, Bajaj R, del Rio C. Emphysematous cholecystitis due to Salmonella derby. Lancet Infect Dis. 2006;6(2):118-120.
doi - Pal K. Laparoscopy in the management of emphysematous cholecystitis and secondary appendicitis in an 11-year-old child with insulin-dependent diabetes mellitus. Afr J Paediatr Surg. 2011;8(2):211-214.
doi pubmed - Bouras G, Lunca S, Vix M, Marescaux J. A case of emphysematous cholecystitis managed by laparoscopic surgery. JSLS. 2005;9(4):478-480.
pubmed - Grayson DE, Abbott RM, Levy AD, Sherman PM. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002;22(3):543-561.
doi pubmed - Miyahara H, Shida D, Matsunaga H, Takahama Y, Miyamoto S. Emphysematous cholecystitis with massive gas in the abdominal cavity. World J Gastroenterol. 2013;19(4):604-606.
doi pubmed - Sunnapwar A, Raut AA, Nagar AM, Katre R. Emphysematous cholecystitis: Imaging findings in nine patients. Indian J Radiol Imaging. 2011;21(2):142-146.
doi pubmed - Delgado-Plasencia L, Gonzalez-Garcia I, Rodriguez-Gonzalez D, Torres-Monzon AE. Pneumomediastinum as a complication of emphysematous cholecystitis: case report. BMC Gastroenterol. 2010;10:99.
doi pubmed - Safioleas M, Stamatakos M, Kanakis M, Sargedi C, Safioleas C, Smirnis A, Vaiopoulos G. Soft tissue gas gangrene: a severe complication of emphysematous cholecystitis. Tohoku J Exp Med. 2007;213(4):323-328.
doi pubmed - Choi HS, Lee YS, Park SB, Yoon Y. Simultaneous emphysematous cholecystitis and emphysematous pancreatitis: a case report. Clin Imaging. 2010;34(3):239-241.
doi pubmed - Stojanovic D, Lalosevic D, Stojanovic M, Caparevic Z, Dosev M, Ilic J. [Emphysematous cholecystitis]. Med Pregl. 2002;55(11-12):529-531.
doi pubmed - Wu JM, Lee CY, Wu YM. Emphysematous cholecystitis. Am J Surg. 2010;200(4):e53-54.
doi pubmed - Safioleas M, Stamatakos MK, Mouzopoulos GJ, Tziortzis G, Chagiconstantinu K, Revenas K. Emphysematous cholecystitis. Review of five cases and report of septic musculoskeletal complications. Chirurgia (Bucur). 2006;101(1):61-64.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
