| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Original Article
Volume 9, Number 2-3, September 2019, pages 22-25
Management of Chest Trauma in a Rural Medical College Hospital
KABM Taiful Alama, b, MD Sumon Rahmana, Sanjeeda Saada
aDepartment of General Surgery, Jahurul Islam Medical College, Bajitpur, Kishoreganj, Bangladesh
bCorresponding Author: Taiful Alam, Department of General Surgery, Jahurul Islam Medical College, Bajitpur, Kishoreganj 2336, Bangladesh
Manuscript submitted June 10, 2019, accepted June 26, 2019
Short title: Management of Chest Trauma
doi: https://doi.org/10.14740/jcs379
| Abstract | ▴Top |
Background: Chest trauma implies trauma to anyone or combination of different thoracic structures. Approximately in one quarter of civilians, trauma deaths are caused by trauma to thorax. Many of these deaths can be avoided by precise clinical diagnosis and immediate management. Most wounds under these situations could be managed conservatively with or without tube thoracostomy. This study aims to assess and analyze the mode of presentation, pattern and management of chest injuries in rural areas.
Methods: One hundred consecutive patients within the period of 14 months with thoracic trauma presenting in emergency department were evaluated.
Results: Most of the patients (87%) were treated conservatively with minor wound repair and medical treatment and 13% patients had been treated with intercostal chest drain. Among these 13% patients, three were referred to higher centers due to massive initial hemothorax and longstanding pneumothorax.
Conclusions: Majority of the chest injury patients can be treated satisfactorily in general surgery unit by conservative management or chest drain.
Keywords: Chest trauma; Conservative; Pneumothorax; Chest drain
| Introduction | ▴Top |
Trauma is the major public health problem around the world as it is associated with high complication rate and death toll in developing and developed countries. Chest plays important roles in respiration and protection of the vital intrathoracic and upper abdominal organs from externally applied force and is composed of the rigid structures like rib cage, clavicle, sternum, scapula and heavy overlying musculature. Chest trauma implies trauma to anyone or combination of different thoracic structures which can arbitrarily be divided into four distinct anatomical regions: chest wall, pleural space, lung parenchyma and the medistinum [1]. Approximately in one quarter of civilians, trauma deaths are caused by trauma to thorax and many of these deaths can be avoided by precise diagnosis and proper management [2]. In thoracic trauma, primary care is directed to the rapid evaluation of extent of injury, estimation of volume of blood loss and its rapid replacement by intravenous transfusion, the recognition of hypoxia and respiratory distress and its correction by assurance of a clear airway, full pulmonary expansion and mechanical support of ventilation when necessary [3]. Most wounds of these structures can be managed non-operatively or by simple techniques such as tube thoracostomy.
Among the causes of thoracic trauma road traffic accidents (RTAs), fall from height, blunt trauma, and stab wounds take the major share. Pre-hospital deaths resulting from thoracic injuries are due to great vessel rupture and exsanguinations, cardiac tamponade [4], tension pneumothorax and bilateral flail chest with deep refractory hypoxia.
This study was conducted to asses and analyze the true presentation, pattern and management of chest injuries in general surgery units of a rural medical college hospital.
| Materials and Methods | ▴Top |
Our study was conducted in Jahurul Islam Medical College Hospital which is a secondary level hospital situated in a remote place of Bangladesh at Bajitpur subdistrict, under Kishoregonj district over the period of 14 months (January 18 - February 19). Cases were selected on the basis of traumatic chest injury and the data were recorded successively. We analyzed patients’ demographic profile, nature and cause of trauma, presenting symptoms, associated injuries, underlying co-morbidities, intervention undertaken, length of hospital stay, duration of tube thoracostomy, duration of ventilatory support, complications, mortality and follow-up.
One hundred consecutive patients with thoracic trauma presenting in emergency department were evaluated. Patients above 6 years of age who presented with chest trauma alone and in combination with other trauma were included in this study.
Investigation included blood complete picture, chest and abdomen X-ray, ultrasound, computed tomography (CT) scan, and blood grouping. All the patients were primarily treated as per ATLS (Advanced Trauma Life Support) protocol. Then definitive interventions were taken according to patients’ need.
No IRB was available in this institution for such study as this one. As for ethical compliance, medical ethics was maintained in this study.
Inclusion criteria
Patients who came to emergency and accident department with chest and associated trauma and who had definitive clinical and radiological findings of chest trauma are included in this study.
Exclusion criteria
Patients who had only mild chest pain following chest trauma, had no clinical or radiological signs are excluded in this study. Severe chest trauma and chest wall defects are excluded in this study.
| Results | ▴Top |
A total of 100 patients were studied for chest traumas during 14 months. The age of patients ranged from 6 to 75 years. Among them, 65% are men and 35% are women. Incidence in our study is almost similar in different age groups with the exception in the sixth decade (Table 1).
 Click to view | Table 1. Distribution of Patients According to Age Group |
RTA was the major cause of chest trauma followed by fall from the height, blunt trauma and others (Table 2).
 Click to view | Table 2. Modes of Injury Is Mentioned in the Table |
Many patients (n = 17) had associated injuries in different parts of the body. Majority of them were treated in the concerned department together with chest trauma management.
Among the associated injury patients head injury patients were on the top of the list (Fig. 1).
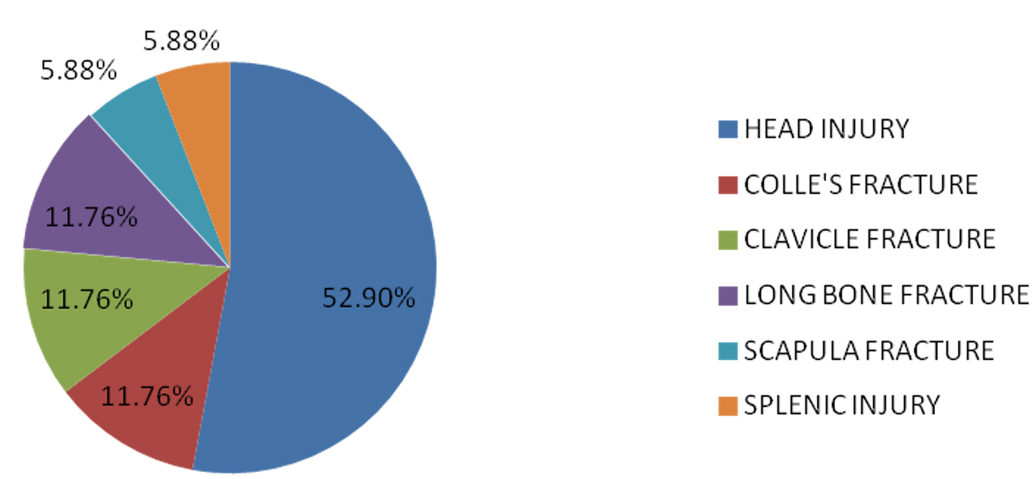 Click for large image | Figure 1. Associated trauma patients. |
Chest wall external wound such as abrasion, bruise, laceration, surgical emphysema with chest pain contributes to 64%. Rest of the patients had single or multiple rib fracture, hemothorax, pneumothorax and hemopneumothorax (Table 3).
 Click to view | Table 3. Modes of Presentation of Patients |
Most of the patients (87%) were treated conservatively with minor wound repair and medical treatment with adequate follow-up. A total of 13% patients (n = 13) were treated with intercostal chest drain (Fig. 2).
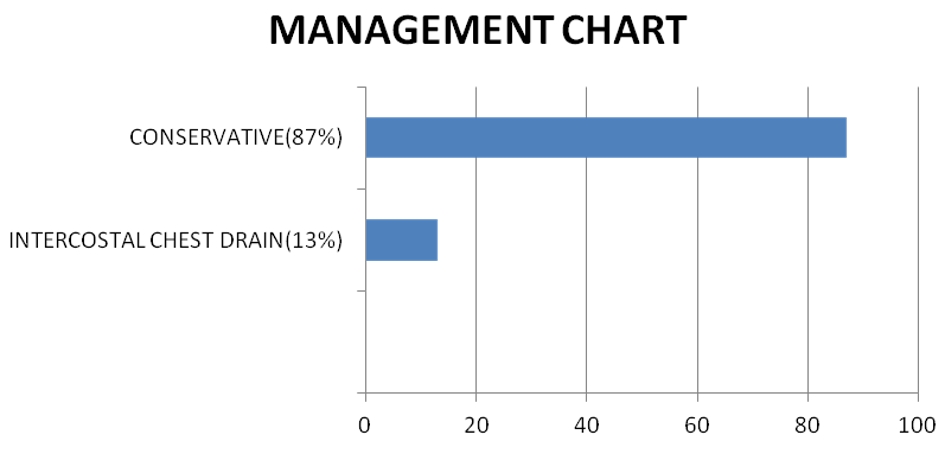 Click for large image | Figure 2. Distribution of patients according to management strategy. |
Out of 13 patients, three were referred to higher centers with longstanding pneumothorax and hemothorax with unstable vital parameters. A total of nine patients were referred to specialized higher centers, six of whom were referred to neurosurgery unit as they suffered from head injury. All of these referred patients received conservative treatment or interventional (chest drain) management in our center.
Hospital stay of the patients was noted as most patients who were treated conservatively stayed for 1 - 3 days and those who were treated with chest drain stayed for 4 - 7 days (Fig. 3).
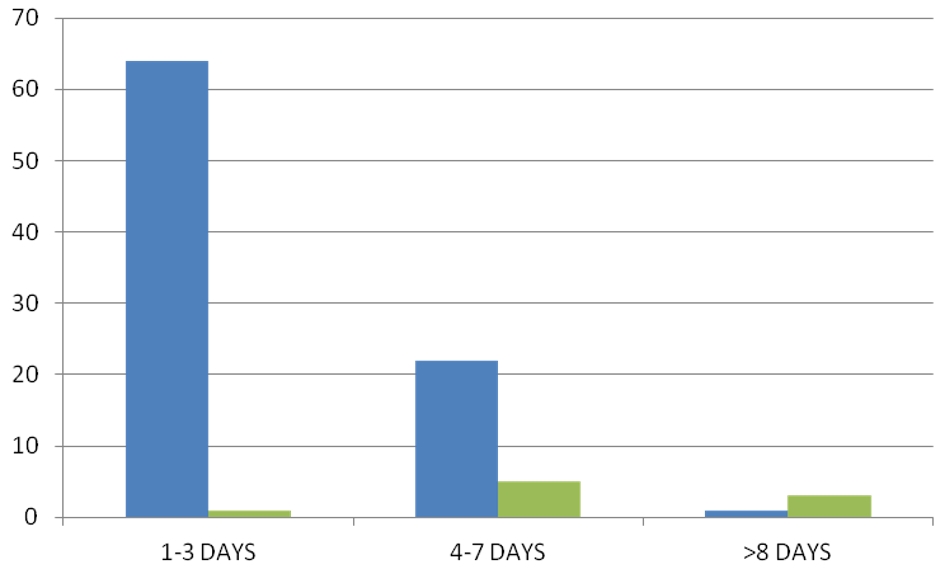 Click for large image | Figure 3. Hospital stay. Blue bar denotes hospital stay of patients having conservative management and green bar denotes hospital stay of patients having interventional management (chest drain). |
In our series a total of 13 patients received intercostal chest drain. Most of the patients (n = 9) had to keep chest drain for 4 - 7 days. One patient was referred to cardiothoracic center on the first POD and three patients had to keep their drain for more than 8 days (Table 4). Among these three patients, two were referred to higher center for progressive pneumothorax.
 Click to view | Table 4. Tube Duration |
Patients who had fractured ribs and intercostal drain were provided with oxygen support and breathing exercise by spirometer as long as they stayed in the hospital. But those patients who had co-morbidities such as chronic obstructive pulmonary disease (COPD), pulmonary tuberculosis (TB) (Table 5) had to keep the oxygen support and breathing exercise for 2 weeks. One patient developed empyema thoracis in follow-up which was further drained by repeat intercostal chest drain. One patient was noticed with kinking of intercostal chest drain tube which was repositioned and properly fixed.
 Click to view | Table 5. List of Patients Having Co-Morbidities |
Another patient developed tube blockage which was irrigated with normal saline and functioned properly. Subcutaneous emphysema was noted in one patient who was improved with conservative management. Surgical site infection was noted in the drain site which delayed wound healing in one patient that needed regular dressing and follow-up.
| Discussion | ▴Top |
As our hospital is located in a rural area, depending on the nature of trauma, most of our patients could be managed conservatively. Conservative management can be applied to patients with mild or small injuries, those who have no other significant injuries and those who are maintaining vital signs and oxygenation. The insertion of a chest tube is therefore not an essential part of the treatment of all chest injuries [5]. Many western studies also suggest that observation or chest tube placement, adequate volume replacement, occasional respiratory support and serial chest X-rays are the only treatment required in 80-85% of the patients [6, 7]. In our study 97% patients were improved with conservative and intercostal chest drain management, which is similar to a study done by Kulshrestha et al [8], in which 96% patients were improved with conservative and intercostal chest drain management.
In our locality there was less availability of high velocity transport, so among the RTA patients no such severe casualty was commonly observed. Literature search is suggestive of RTAs as the main cause of chest injuries worldwide, more so in the developing countries [9]. Our study shows that RTA is also the main cause of chest injury. Head injury is described as the most common associated injury in most of the studies [10]. In this study head injury is also the most common associated injury (52.94%).
The most common presentation in our study is minor chest wall injury with chest pain followed by rib fracture though in all other studies fracture of ribs are the most common thoracic injury followed by lung contusion [11]. As our hospital is not equipped with casualty ward so all the patients who sustained thoracic injury got themselves admitted to surgery ward and are included in this study. This is why chest wall injury superseded all other injuries in this study. Only 4% patients had penetrating (stab) injury, among whom one patient developed massive hemothorax and was referred to higher center for definitive management. Incidence of hemothorax is low (1%) in our study, which is comparable (3.3%) to a study done by Shorr et al [12]. In this study 20% patients have pleural collection (i.e. hemothorax, pneumothorax or hemopneumothorax), and thirteen of them are treated with intercostal chest drain and the rest seven have been improved with conservative management. Patients having mild pneumothorax are observed, analgesic, antibiotic and chest physiotherapy were given, and clearance of bronchial secretions and vital signs are monitored. They do not have any respiratory distress and repeat chest X-ray does not show any further expansion of size of pneumothorax. So they are not provided with intercostal chest drain. Pramod et al suggest that some traumatic pneumo/hemothorax will resolve spontaneously when managed conservatively [13]. In a large South African series of predominantly penetrating injuries to the chest [14], traumatic pneumothorax was initially managed conservatively if there was < 20% reduction in lung volume.
A chest tube is compulsory for patients in respiratory distress on presentation, patients who require invasive positive pressure ventilation (IPPV), those with associated significant injuries, and those who develop respiratory distress during conservative management.
Conclusions
In a rural secondary level hospital majority of the chest injury patients can be treated satisfactorily in a general surgical unit by conservative management or by insertion of chest drain into the pleural cavity and few patients who need major surgery like thoracotomy should be transferred to higher centre.
RTA: road traffic accident.
Acknowledgments
We are grateful to Dr. A. K. M. Maruf Raja, Associate Professor of Pathology, Jahurul Islam Medical College for his suggestion to publish this article in this journal. We are also grateful to our clinical assistant and radiologist.
Financial Disclosure
There was no institutional funding for this study.
Conflict of Interest
There is no conflict of interest among the authors.
Informed Consent
Informed consent was taken from all patients or their guardians.
Author Contributions
TA contributed to study planning, conduction and analysis; SR was involved in preparing tables and figures and designing; SS contributed to selection of cases and collection of data.
| References | ▴Top |
- Hoyt DB, Coimba R, Engthelhaardt S, Hansbrough JF, Steele RJC, Moosa AR, (ed). Essential surgical practice. 4th ed. London: Arnold; 2002. p: 5-15.
- Dalal S, Nityasha VM, Vashisht M, Dahiya R. Prevalance of chest trauma at an Apex institute of North India. A retrospective study. Internet J Surg. 2008;18:1.
doi - Vigar VS, Solanki MI. Analytic study of chest injury. IJSS Journal of Surgery. 2015;1(1):5-9.
- May AK, Patterson MA, Rue LW, 3rd, Schiller HJ, Rotondo MF, Schwab CW. Combined blunt cardiac and pericardial rupture: review of the literature and report of a new diagnostic algorithm. Am Surg. 1999;65(6):568-574.
- Johnson G. Traumatic pneumothorax: is a chest drain always necessary? J Accid Emerg Med. 1996;13(3):173-174.
doi pubmed - Bastos R, Baisden CE, Harker L, Calhoon JH. Penetrating thoracic trauma. Semin Thorac Cardiovasc Surg. 2008;20(1):19-25.
doi pubmed - Robison PD, Harman PK, Trinkle JK, Grover FL. Management of penetrating lung injuries in civilian practice. J Thorac Cardiovasc Surg. 1988;95(2):184-190.
- Kulshrestha P, Iyer KS, Das B, Balram A, Kumar AS, Sharma ML, Rao IM, et al. Chest injuries: a clinical and autopsy profile. J Trauma. 1988;28(6):844-847.
doi pubmed - El-Menyar A, Abdelrahman H, Al-Hassani A, Ellabib M, Asim M, Zarour A, Al-Thani H. Clinical presentation and time-based mortality in patients with chest injuries associated with road traffic accidents. Arch Trauma Res. 2016;5(1):e31888.
doi pubmed - Pearson FG, Joel O, Deslauriers CJ, Patterson A, Cooper JD. Thoracic Surgery. 2nd ed. Philadelphia, PA: Churchill Livingstone; 2002.
- Unsworth A, Curtis K, Asha SE. Treatments for blunt chest trauma and their impact on patient outcomes and health service delivery. Scand J Trauma Resusc Emerg Med. 2015;23:17.
doi pubmed - Shorr RM, Crittenden M, Indeck M, Hartunian SL, Rodriguez A. Blunt thoracic trauma. Analysis of 515 patients. Ann Surg. 1987;206(2):200-205.
doi pubmed - Pramod T, C A Shashirekha CA, Chandan KR, Harsha R. Role of conservative management of traumatic chest injuries: a retrospective study & review of literature. International Journal of Scientific Study. 2015;3(8):147-150.
- Knottenbelt JD, van der Spuy JW. Traumatic pneumothorax: a scheme for rapid patient turnover. Injury. 1990;21(2):77-80.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
