| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Original Article
Volume 9, Number 4, December 2019, pages 45-50
Analysis of Transfusion Volumes in the Elderly Trauma Population
Manrique Alberto Guerreroa, b, Monica Sridhara, Stephanie Yeea, Jacob Millera, Jafar Haghshenasa, Jamshed Zuberia, Robert Madlingera
aSurgery Department, St. Joseph’s University Medical Center, Paterson, NJ, USA
bCorresponding Author: Manrique Alberto Guerrero, Surgery Department, St. Joseph’s University Medical Center, Paterson, NJ, USA
Manuscript submitted October 7, 2019, accepted October 30, 2019
Short title: Blood Transfusion in Elderly Traumas
doi: https://doi.org/10.14740/jcs392
| Abstract | ▴Top |
Background: Blood transfusion and old age have been independently associated with worse outcomes and higher mortality in the trauma population. Determining specific volumes and ratios of blood products for the elderly population, a special population with varied hemodynamic responses to traumatic injury, is a challenge. This study was aimed at delineating the relationship between specific transfusion volumes and mortality with an ultimate goal of finding an optimal threshold where risk outweighs benefit.
Methods: A retrospective study of data from patients aged 65 and older at a level II urban trauma center was conducted. All patients who were included in the study presented to the emergency department between January 2013 and January 2016 and received a blood product transfusion (n = 93). The primary outcome was defined as mortality 24 h after transfusion, while the secondary outcome measured was length of hospital stay. Optimal cut-off points were estimated using Youden J coefficients, and Cox proportional hazard ratio (HR) was performed to calculate mortality risk.
Results: Patients receiving less than 5 units of blood product had a shorter length of stay (5.19 days) and decreased risk of mortality (HR = 2.48, P = 0.01). Patients receiving ≥ 5 units of a blood product had a statistically significant increase in risk of mortality (HR = 6.207, P < 0.001) and length of hospital stay (12.47 days), regardless of injury severity score. The administration of fresh frozen plasma was also an independent predictor of mortality. Patients who received a plasma transfusion had an increased risk of mortality (HR = 3.25, P < 0.001).
Conclusion: In this study, a threshold point of greater than 5 units of blood products has been associated with increased mortality and length of hospital stay. A more restrictive transfusion strategy has potential for improved outcomes.
Keywords: Retrospective study; Transfusion volume; Elderly trauma; Threshold volume; Restrictive transfusion strategy; Liberal transfusion strategy; Blood products
| Introduction | ▴Top |
The US aging population is rapidly growing. According to the United States Census Bureau, residents aged 65 and older grew from 35.0 million in 2000 to 49.2 million in 2016, accounting for 12.4% and 15.2% of the total population, respectively [1]. Elderly trauma specifically accounts for nearly 23% of all trauma admissions and one-third of all injury-related deaths [2]. When compared to the younger population, geriatric trauma patients have greater morbidity and mortality, longer hospital stays and increased usage of hospital resources [3]. Therefore, it is important to understand the proper management of the geriatric trauma population.
Currently, transfusion guidelines in the elderly trauma population have been a contested topic among many physicians, due to the complex physiological nature of elderly patients. Studies focused on the elderly trauma population have shown that older age and massive transfusions independently increase the risk of mortality and worse outcomes in the trauma population and have therefore supported more restrictive transfusion strategies [4-8]. Conversely, meta-analysis and systematic reviews have shown that liberal transfusions might produce better outcomes in the geriatric population compared to restrictive transfusion strategies [9]. In this study, a retrospective review was conducted to delineate the relationship between specific transfusion volumes and mortality, with the goal of finding an optimal threshold where risk outweighs benefit. It was hypothesized that a restrictive transfusion approach would lead to a decreased mortality when compared to a more liberal transfusion approach.
| Materials and Methods | ▴Top |
This study was a single-center retrospective observational study of elderly trauma patients who received blood transfusion at a level II urban trauma center, between January 2013 and January 2016. Data were acquired from the hospital’s trauma registry. The study was IRB approved and patient consent was waived due to the observational nature of the study. A total of 1,186 elderly patients presented to the emergency department and the patients’ age, sex, mechanism of injury, length of hospital stay (LOS), quantity and type of blood products, injury severity score (ISS) and mortality status were recorded and reviewed. Patients who expired or were discharged within 24 h of presentation to the trauma bay were excluded from the study. Patients were defined as having received a transfusion if they received packed red blood cells (PRBCs), fresh frozen plasma (FFP), platelets, or any combination of the aforementioned blood products during any point of their hospital stay; a total of 93 patients received blood products. Hospital mortality after 24 h from admission was measured as the primary outcome. The secondary outcome was LOS.
Analysis was performed using Stata 15. In order to detect skewness and kurtosis in the multivariate setting, the Doornik-Hansen test was carried out. The test was shown to follow a parametric distribution. Due to adherence of a parametric distribution, significant differences between survivors and non-survivors as well as group demographics were assessed using a Student’s t-test. Categorical variables were assessed using χ2. Powerwise correlation using Bonferroni adjustment was used to determine significant variable interactions. In order to determine optimal cut-off points of blood product volumes, Youden J coefficients were used. To define the independent predictors of mortality, Cox proportional hazard ratio (HR) was calculated to assess the mortality risk in patients with specific transfusion volumes and to assess the mortality risk in patients with specific blood product transfusion. Regression analysis was used to determine LOS as a secondary outcome. Analysis was performed for the entire patient population and repeated based off stratification. A P-value of < 0.05 was considered significant.
| Results | ▴Top |
Between January 2013 and January 2016, 1,186 patients, greater than 65 years of age, were admitted. Ninety-three patients, composed of 56 females (60%) and 37 males (40%), received blood products and met the inclusion criteria. Transfusion patients had a mean age of 77.73 years (range 65 - 101 years, standard deviation (SD) 8.32 years), an average LOS of 8.80 days (range 1 - 37 days, SD 8.60 days) and an average of 3.73 units of total blood products (range 1 - 20 units, SD 4.05 units) given. Of the injuries, 92.47% in the transfused patient population were penetrating with an average ISS of 19.13 (range 1 - 75, SD 10.47). Overall, 35 (38%) of the elderly transfusion trauma patients died, while 58 (62%) of the transfusion patients survived. Using the Youden J coefficients, a transfusion volume of 5 units was found to be the threshold value, where risk outweighed benefit. Of the 58 patients who survived, 87.94% of patients received less than 5 units of blood products, while 12.06% of the patients received ≥ 5 units of blood products. Conversely, of the 35 patients who did not survive, 44.29% received less than 5 units of blood products, while 45.71% received ≥ 5 units of blood products.
Table 1 shows that LOS, receiving FFP, number of units given and ISS were significantly different when comparing survivors with non-survivors.
 Click to view | Table 1. Characteristics of Transfused Elderly Trauma Patients |
Multiple Cox proportional analysis was performed to highlight independent predictors of mortality in the study group (Table 2).
 Click to view | Table 2. Cox Proportional Analysis: Independent Predictors of Mortality |
The number of units received, FFP and ISS were found to be independent predictors of mortality (Table 2). Although age and gender were in the threshold of being significant as independent predictors of mortality within the general population, they lost their significance when analyzed in the transfusion population (Table 1).
Patients that received ≥ 5 units of blood transfusion were shown to have increased mortality risk, with an HR of 6.27 (confidence interval (CI) 3.62 - 10.88), compared to those who received < 5 units of blood transfusion, with an HR of 2.48 (CI 1.46 - 4.20) (Table 3 and Fig. 1). Both of these groups had significantly higher risk of mortality when compared to those who received no transfusion. The ISSs between the two transfusion groups were 18.63 for < 5 units and 22.22 for ≥ 5 units, with a P value of 0.15 (Table 4).
 Click to view | Table 3. Hazard Ratio for Transfusion Groups |
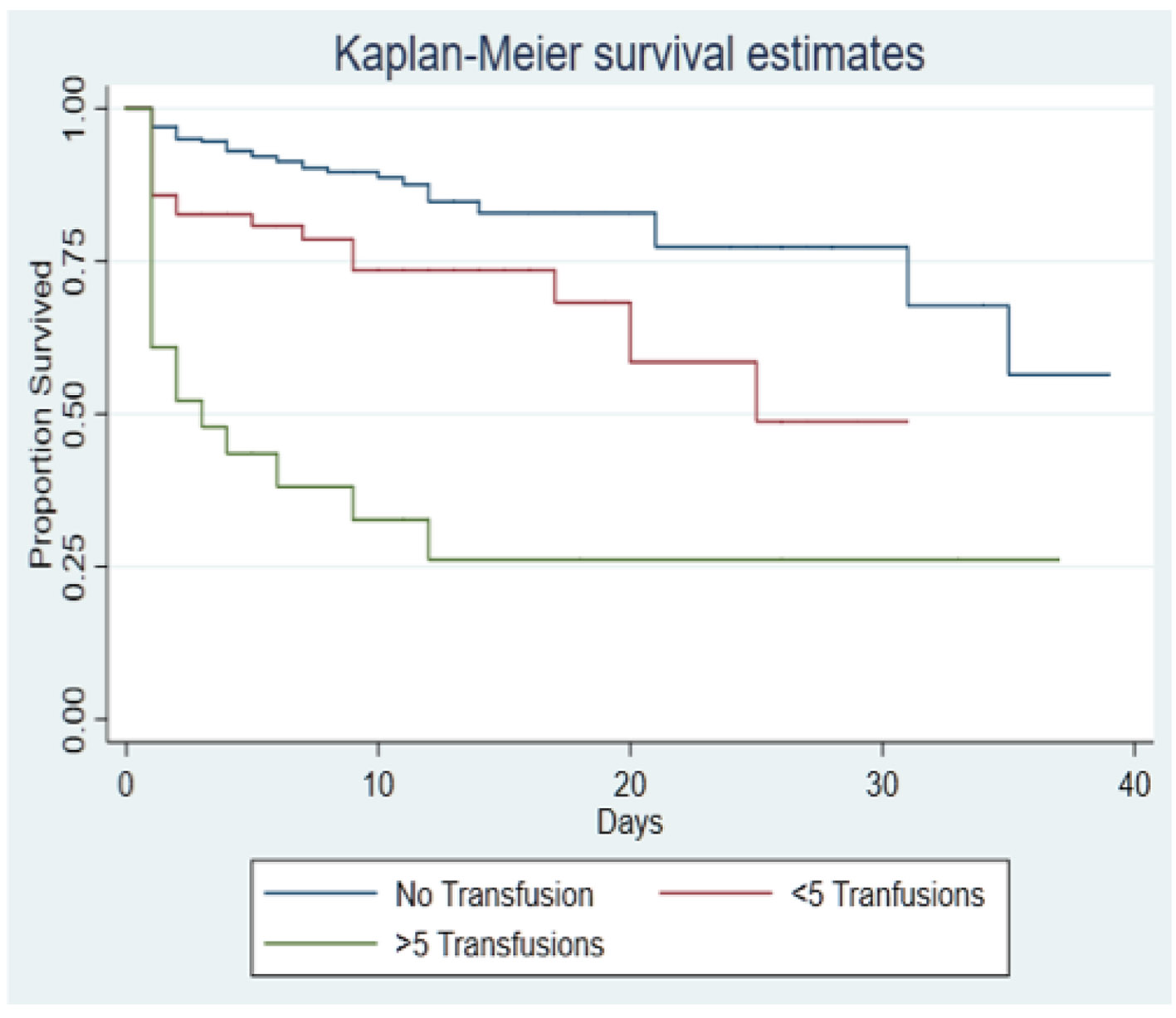 Click for large image | Figure 1. Kaplan-Meier 40-day survival curves according to transfusion volume. |
 Click to view | Table 4. ISS Stratified by Transfusion Group |
Our secondary outcome, LOS was found to be statistically different between the two groups (Table 5). Patients who received < 5 units had an average stay of 5.19 days (P < 0.001) compared to average stay of 12.47 days for those who received ≥ 5 units (P < 0.001).
 Click to view | Table 5. LOS Based on Transfusion Volume |
Receiving FFP was also found to be statistically different between the two transfusion groups (Table 1) and an independent predictor of mortality (Table 2). FFP was found to have a corresponding HR of 3.25 (CI 1.91 - 5.53, P < 0.001) (Table 6 and Fig. 2).
 Click to view | Table 6. Hazard Ratio |
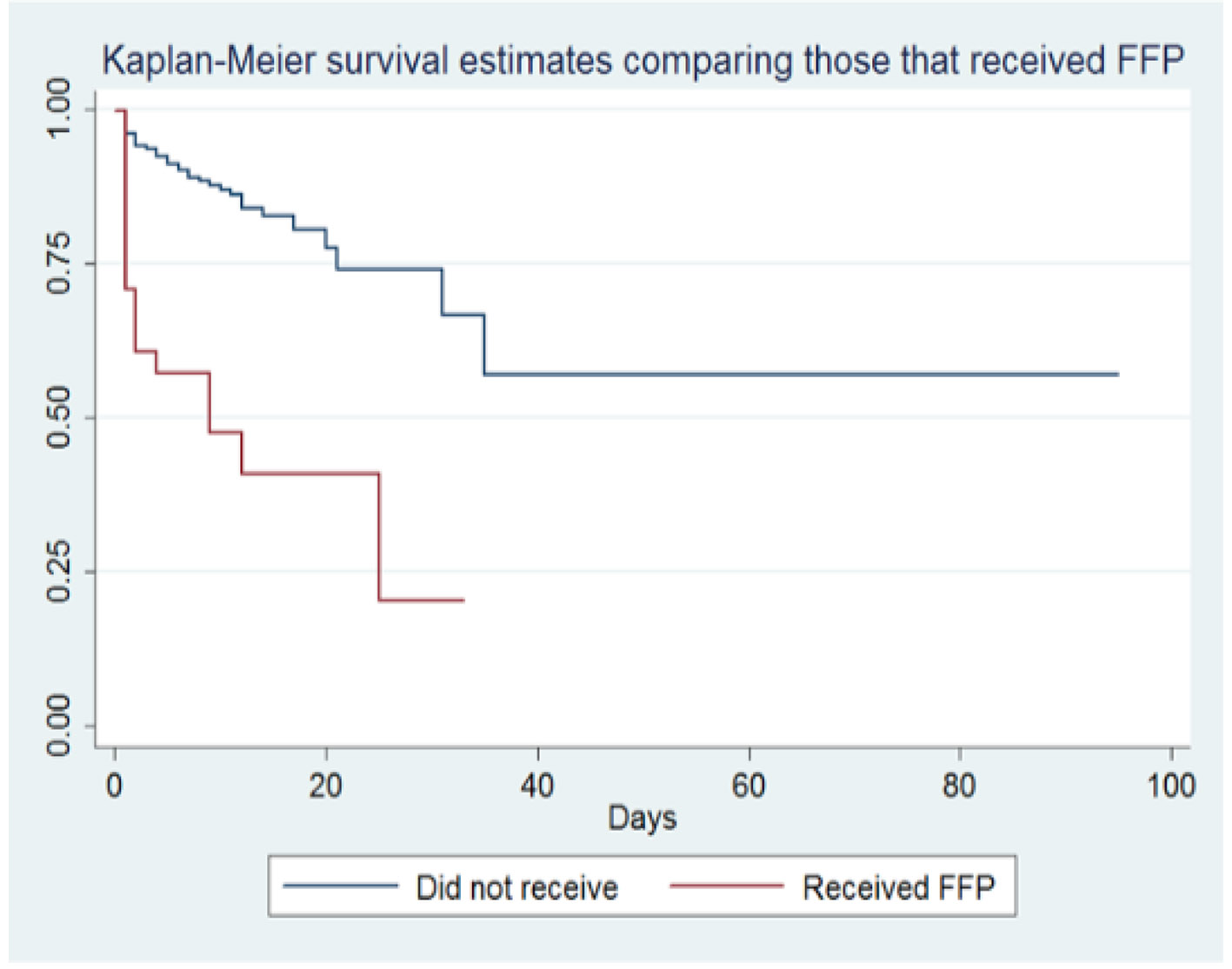 Click for large image | Figure 2. Figure 2. Kaplan-Meier 100-day survival curves according to FFP transfusion. FFP: fresh frozen plasma. |
| Discussion | ▴Top |
Blood transfusion protocol has been a contested topic for many years, especially in the elderly patient population. Blood products carry their own mortality risks with increased inflammatory markers, coagulopathy, immunosuppression and infection potential. In addition, elderly patients carry their own mortality risks, such as a delicate physiology and increased comorbidities. Clinical protocols and literature have argued for both restrictive and liberal transfusion protocol for elderly trauma patients, making it difficult to decipher best practice for this patient population.
Some literature supports a more restrictive transfusion protocol. Mostafa et al, in his retrospective review of patients who received blood transfusion in the first 24 h after injury, indicated higher mortality risk with increased PRBC transfusion volume in elderly patients when compared to the younger population [10]. Their analysis demonstrated that the mean packed cell transfusion volume for all survivors decreased significantly with age [10]. Furthermore, Veenith et al indicated in their research similar results [11]. Their retrospective cohort study demonstrated increased duration of stay in the intensive care unit and increased odds ratio of mortality with increased transfusion amounts after considering EuroSCORE and body mass index for elderly patients following cardiac surgery [11].
Conversely, other studies support a more liberal resuscitation approach. Mitra et al, in a retrospective review in a level I trauma center, demonstrated in their analysis a total of 20 (39.2%) deaths in an elderly massively transfused patient population compared to 55 (21.1%) deaths among younger massively transfused patients [12]. These results counteract a restrictive transfusion strategy, instead demonstrating survival to hospital discharge in elderly patients receiving massive transfusions after trauma despite the mortality risks. Simon et al in their systematic review and meta-analysis similarly agreed that liberal transfusion strategies might produce better outcomes in geriatric patients than restrictive transfusion strategies [13].
Our retrospective study at a level II trauma center furthers this discussion by focusing on the effect of blood transfusion volume on elderly trauma patients, in terms of mortality and LOS. Specifically, our study wanted to explore a threshold value of blood products, where risk outweighed benefit, a topic not previously researched in other studies.
Using the Youden J coefficients, a threshold value of 5 units of blood products was found to be the cut-off value where there was an increased mortality risk and LOS. When comparing survivors with non-survivors in the transfused patient population, 12.06% of survivors compared to 45.71% of non-survivors received ≥ 5 units of blood products with a P value of < 0.001.
ISS could affect the amount of blood products given. Our study, however, took this into account and our analysis consistently showed that 5 units of blood products had an almost three times increase in mortality risk regardless of ISS (Table 4) and an almost over two times increase in LOS when compared to those who received < 5 units. LOS is of serious concern in the healthcare field. An increase in LOS increases the risk for hospital-acquired infections, cost and other complications among patients, prompting clinicians to reduce hospital days across the board when possible.
Furthermore, these results support the concept that elderly patients have a delicate physiology and that even a small amount of transfusion volume could increase the risk for adverse outcomes. Although 5 units is not the absolute cut-off value for transfusion when it comes to the elderly population, this study continues the conversation of being more conservative when it comes to giving blood products to elderly trauma patients. Receiving FFP was also found to be an independent predictor of mortality and had a significantly increased HR when compared to those who did not receive FFP. This result should be considered in light of current increased use of novel anticoagulants in elderly patients, pushing more FFP to be given during transfusion. Furthermore, the increased use of novel anticoagulants due to medical conditions, such as cardiac disease, raises the potential to study the effect of comorbidities on transfusion volume and mortality in future studies. Another potential for future studies takes into consideration pre-existing coagulopathy prior to transfusion. As no point-of-care mechanism exists in the trauma setting, it is difficult to determine if coagulopathy is apparent. Some centers use thromboelastography as a method to assess potential coagulopathy in patients. Future research could be aimed at using these quantifiable values in further elucidating guidelines in trauma management. Lastly, transfusion triggers should also be considered in future studies. Future studies should analyze baseline hemoglobin and hematocrit, lactate levels, blood pressure, central venous oxygen saturation and base deficit prior to transfusion and see their effects on amount of blood products given and consequently mortality.
Our study has certain limitations and weaknesses. There was a relatively small transfusion population studied (n = 94). Timetable of transfusion should also be looked at, specifically when the products were administered and how that affected mortality. Furthermore, our data are only generalizable to patients over 65 years of age and we did not consider other comorbidities. While there is a correlation between FFP and mortality, we cannot determine a causal relationship. A randomized, case-matched study could be designed to tease out this relationship.
Conclusions
Our study showed that patients who received ≥ 5 units of blood products had an increased risk of mortality regardless of ISS and an increased LOS. Receiving FFP was also found to be an independent predictor of mortality.
Clinical significance
When it comes to the debate of liberal versus restrictive transfusion strategies, especially when it comes to elderly trauma patients, our study’s results overall support a more restrictive transfusion strategy.
Acknowledgments
St. Joseph’s University Medical Center.
Financial Disclosure
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Conflict of Interest
Authors report no conflict of interest.
Informed Consent
Patient consent was waived due to the observational nature of the study.
Author Contributions
Dr. Manrique Guerrero collected data and wrote the paper. Dr. Monica Sridhar helped collect data, conceived and designed the analysis. Dr. Stephanie Yee helped collect the data and write the paper, including revisions and formatting. Dr. Jacob Miller performed the analysis. Dr. Jafar Haghshenas helped collect data, perform analysis and edit paper. Dr. Jamshed Zuberi edited paper. Dr. Robert Madlinger edited paper.
| References | ▴Top |
- U.S. Census Bureau, Population Division, Annual estimates of the resident population for selected age groups by sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2014. Release date: June 2015.
- National hospital ambulatory medical care survey: 2011 emergency department summary tables. Table 2, 7.
- Mitra B, Cameron PA. Optimising management of the elderly trauma patient. Injury. 2012;43(7):973-975.
doi pubmed - Sisak K, Manolis M, Hardy BM, Enninghorst N, Bendinelli C, Balogh ZJ. Acute transfusion practice during trauma resuscitation: who, when, where and why? Injury. 2013;44(5):581-586.
doi pubmed - DeLeon AN, Uecker JM, Stafford SV, Ali S, Clark A, Brown CV. Restrictive transfusion in geriatric trauma patients. Am Surg. 2016;82(1):85-88.
- Murry JS, Zaw AA, Hoang DM, Mehrzadi D, Tran D, Nuno M, Bloom M, et al. Activation of massive transfusion for elderly trauma patients. Am Surg. 2015;81(10):945-949.
- Keuter K, Ablah E, Vasquez D, Wetta-Hall R, Hawley SR. Blood transfusions in elderly trauma patients: is there a role for restrictive use? J Am Geriatr Soc. 2008;56(1):168-170.
doi pubmed - Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340(6):409-417.
doi pubmed - Ohmori T, Kitamura T, Tanaka K, Saisaka Y, Ishihara J, Onishi H, Nojima T, et al. Bleeding sites in elderly trauma patients who required massive transfusion: a comparison with younger patients. Am J Emerg Med. 2016;34(2):123-127.
doi pubmed - Mostafa G, Gunter OL, Norton HJ, McElhiney BM, Bailey DF, Jacobs DG. Age, blood transfusion, and survival after trauma. Am Surg. 2004;70(4):357-363.
- Veenith T, Sharples L, Gerrard C, Valchanov K, Vuylsteke A. Survival and length of stay following blood transfusion in octogenarians following cardiac surgery. Anaesthesia. 2010;65(4):331-336.
doi pubmed - Mitra B, Olaussen A, Cameron PA, O'Donohoe T, Fitzgerald M. Massive blood transfusions post trauma in the elderly compared to younger patients. Injury. 2014;45(9):1296-1300.
doi pubmed - Simon GI, Craswell A, Thom O, Fung YL. Outcomes of restrictive versus liberal transfusion strategies in older adults from nine randomised controlled trials: a systematic review and meta-analysis. Lancet Haematol. 2017;4(10):e465-e474.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
