| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Case Report
Volume 2, Number 3, June 2012, pages 113-115
Breast MRI as a Problem Solving Tool in Paget’s Disease of the Nipple
Gudrun Petersa, e, Mary Selfb, Anne Lynchc, Lynne Brothersd
aRegional Imaging Tasmania, 49 Augusta Road, Lenah Valley 7008 TAS, Australia
bRoyal Hobart Hospital, 48 Liverpool Street, Hobart 7000 TAS, Australia
cBreast Imaging Victoria, Level 2, 166 Gipps St, East Melbourne VIC 3002, Australia
dWomen’s Imaging, 18 Main Road, Moonah 7009 TAS, Australia
eCorresponding author: Gudrun Peters
Manuscript accepted for publication June 7, 2012
Short title: Breast MRI
doi: https://doi.org/10.4021/jcs80w
| Abstract | ▴Top |
Paget’s disease of the nipple is a rare breast malignancy. It is usually, but not always, associated with an underlying ductal carcinoma in situ or invasive ductal carcinoma. Conventional breast imaging studies often fail to detect underlying breast malignancy when present. The following article will discuss the role of breast MRI as a problem solving tool in Paget’s disease of the nipple-areolar complex in patients with no abnormality on clinical examination and normal mammography.
Keywords: Paget's disease nipple areolar complex; Breast; MRI
| Introduction | ▴Top |
Paget’s disease of the nipple is a rare malignancy of the breast accounting for 2% to 3% of breast cancers [1, 2]. It is characterized by infiltration of the nipple-areolar complex by adenocarcinoma cells [1, 3]. Clinically, patients present with eczematous changes of the nipple. If Paget’s disease is suspected, a skin punch biopsy is performed to obtain a diagnosis. Often, but not always, Paget’s disease of the nipple is associated with underlying ductal carcinoma in situ (DCIS) or an invasive ductal carcinoma and the underlying malignancy is in the majority of cases contiguous with Paget’s disease of the nipple [2-4]. Conventional imaging may not detect an underlying malignancy in as many as 65% of cases [4]. More recently, breast MRI has been identified as a modality which may improve detection of clinically and mammographically occult breast malignancies associated with Paget’s disease [2-5]. We present a case of confirmed Paget’s disease of the nipple with no abnormality on clinical examination and a normal mammogram. The role of breast MRI as a decision making tool in treatment planning is discussed.
| Case Report | ▴Top |
A 58 year old woman was referred for diagnostic workup of biopsy-proven Paget’s disease of the nipple-areolar complex. The patient had a history of an open excision biopsy for microcalcification in the right upper inner quadrant 2 years prior to the current presentation with Paget’s disease. Amongst benign breast changes a 2 mm focus of high grade ductal carcinoma in-situ was found. She was otherwise healthy and in particular, had no other known malignancy.
Annual surveillance breast imaging with mammography between 2010 and her presentation with Paget’s disease had been normal apart from post-surgical changes. She had a repeat mammogram at the time of referral, showing no evidence of suspicious microcalcification, architectural distortion or mass lesions. Ultrasound of the right breast was normal. After discussion with the referring breast surgeon, breast MRI was performed for further assessment.
MR imaging
The MRI study was undertaken on a 1.5T Magnetom Espree scanner (Siemens, Erlangen, Germany) with a dedicated 8 channel breast coil. T1-weighted coronal pre-contrast images were obtained to assess the axillary and supraclavicular lymph nodes (repetition time: 483 ms, echo time: 13 ms, slice thickness: 4 mm). Pre-contrast T2-weighted turbo spin echo sequences were also carried out (repetition time: 5030 ms, echo time: 117 ms, slice thickness: 3 mm). A dynamic T1-weighted study with fat suppression before and four times after administration of 0.1 mmol kg-1 of gadolinium-DTPA was performed (repetition time: 4.73 ms, echo time: 1.83 ms, slice thickness: 1.2 mm, acquisition time per sequence 90 s). Post processing procedures included obtaining subtraction images and multiplanar reconstructions (MPR).
The MRI scan showed unilateral nipple enhancement on the right in keeping with the biopsy-proven Paget’s disease of the nipple. There was no mass-like enhancement, but unilateral non-mass-like enhancement was noted in the outer central right breast, prepectoral region (Fig. 1). Given the known right nipple Paget’s disease, it was considered prudent to perform an MRI-guided biopsy of the non-mass-like enhancement. The biopsy was carried out with a SenoRx EnCor breast biopsy system (Bard Biopsy Systems-Tempe, AZ) (Fig. 2). Twelve 10G samples were retrieved and a marker deployed. A post biopsy scan confirmed a cavity in the area of concern (Fig. 3). Histopathology showed benign proliferative breast disease including adenosis, and no evidence of malignancy.
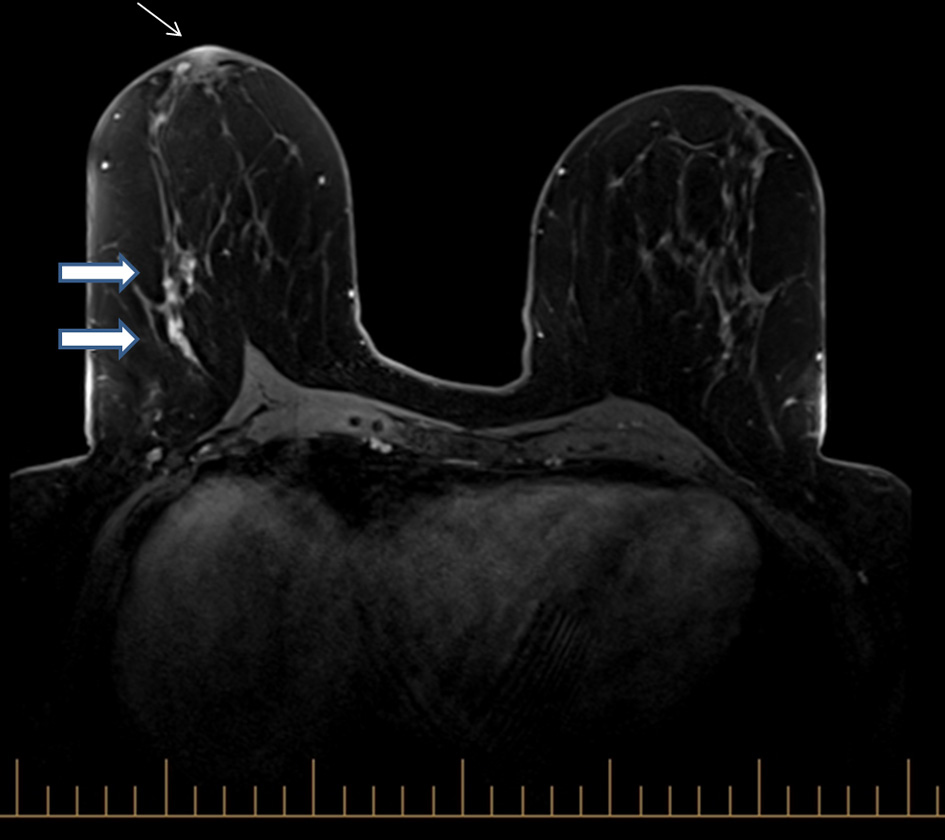 Click for large image | Figure 1. Axial fat-supressed T1-weighted image showing non-mass-like enhancement in the outer central right breast, prepectoral region (large arrows) and unilateral nipple enhancement on the right, in keeping with the known diagnosis of Paget’s disease of the nipple (small arrow). |
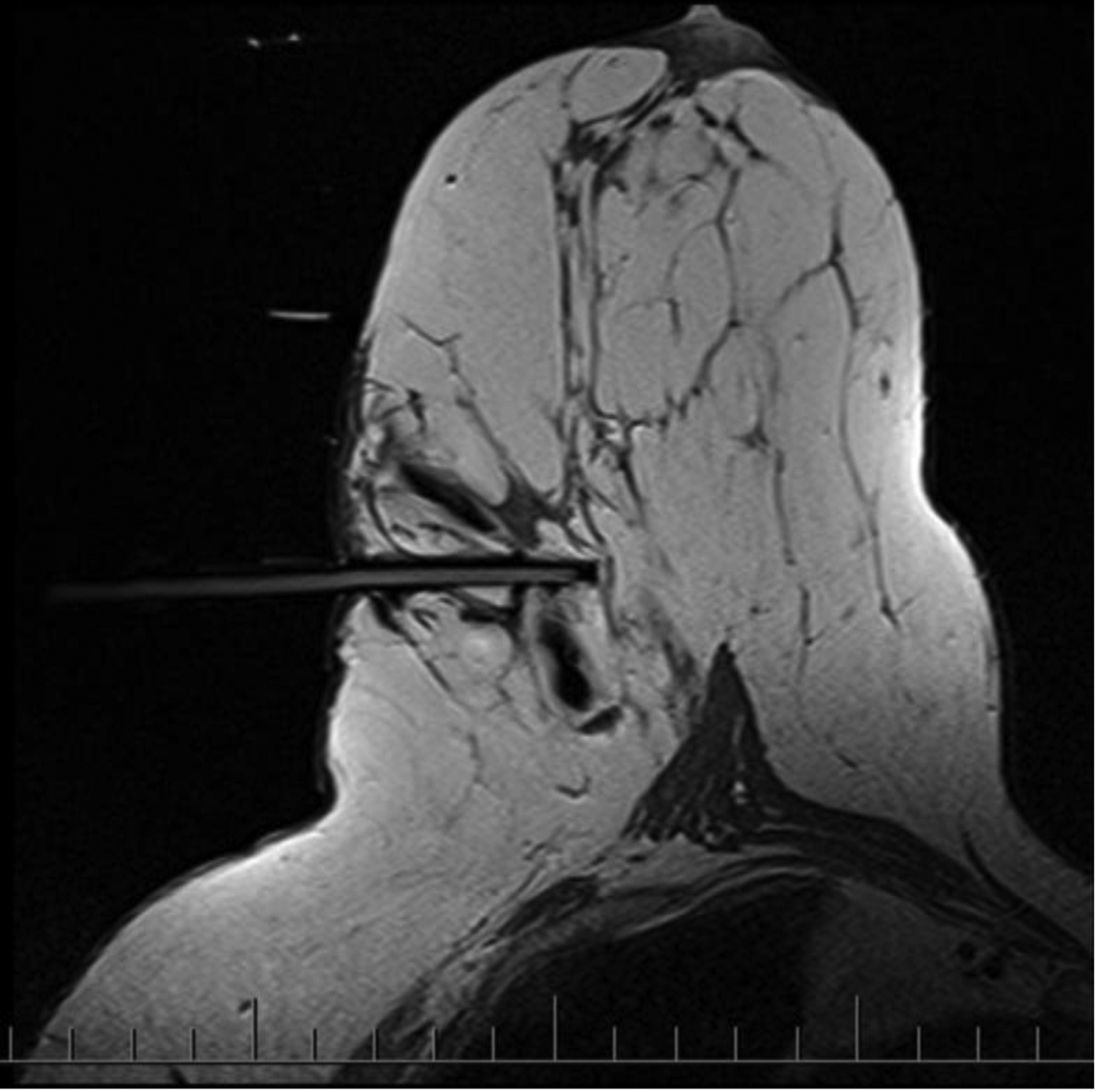 Click for large image | Figure 2. Axial non-fat-supressed T1-weighted image with MRI visible obturator in position, confirming correct needle position. |
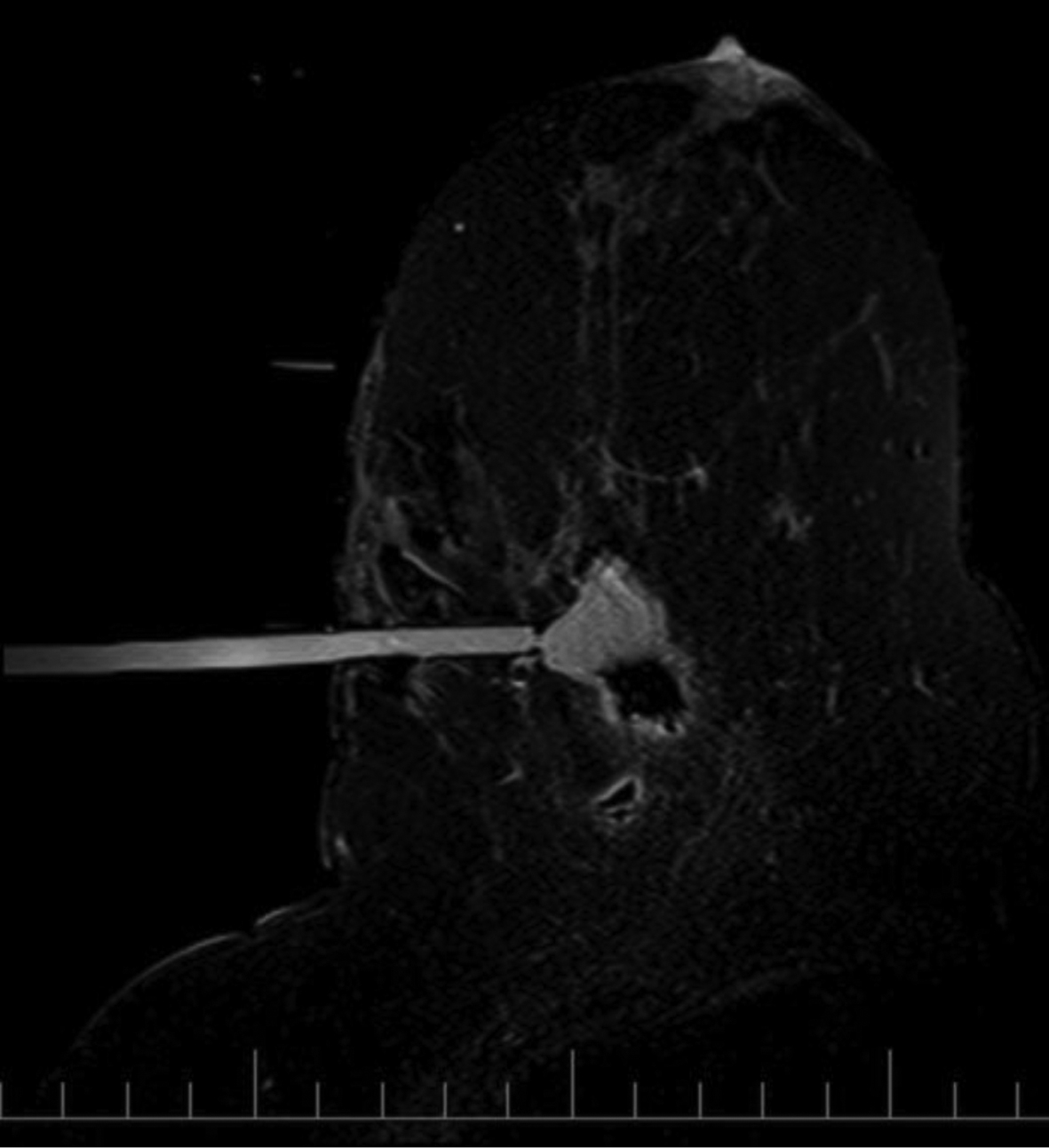 Click for large image | Figure 3. Axial fat-supressed T1-weighted image post biopsy confirms a cavity in the area of previous non-mass like enhancement in the outer central right breast, prepectoral region. |
The patient is now scheduled for breast-conserving surgery.
| Discussion | ▴Top |
Paget’s disease of the nipple accounts for approximately 2% to 3% of breast malignancy [1, 2]. Planning appropriate treatment for Paget’s disease has historically posed a challenge for surgeons because there is a high rate (67-100% of cases) of associated underlying malignancy in [3], which is frequently occult on mammography and ultrasound. Similarly, the absence of a palpable mass in Paget’s disease may indicate the absence of underlying breast malignancy, but more likely indicates that disease is confined to the ductal system (DCIS) [2]. Recently, breast MRI has emerged as a staging tool that can detect otherwise occult malignancy in these patients [1, 2, 3, 5].
Although breast MRI is known to have very high sensitivity in this clinical setting, false positive findings can also occur resulting in a lower specificity [6-8]. In patients with newly diagnosed breast malignancy, including Paget’s disease of the nipple, any asymmetric enhancement should be considered suspicious for further disease [2], and an MR-guided biopsy should be performed to obtain a tissue diagnosis if not seen on a “second-look” ultrasound. In particular, an MRI finding of unilateral non-mass-like enhancement with segmental or ductal distribution and granular internal enhancement is suspicious for associated DCIS [9]. Unfortunately, non-mass-like enhancement is also the major cause of false positive MR findings [7]. In this case, unilateral non-mass-like enhancement away from the nipple on the affected side prompted MRI-guided biopsy. Histology showed benign proliferative breast disease, which was considered concordant with MRI appearances as it is a known MRI mimic of DCIS. Excluding an associated underlying malignancy provided the referring surgeon in this case with important diagnostic information, and allowed appropriate treatment planning.
Conclusion
Paget’s disease of the nipple-areolar complex is a rare breast malignancy with a high rate of associated underlying disease, in which conventional breast imaging with mammography and ultrasound is often normal. Breast MRI is useful as an additional staging tool in this setting, to detect otherwise occult associated ductal carcinoma in situ or invasive malignancy. Breast MRI is also able to exclude underlying malignancy in Paget’s disease, so that breast conservation surgery can be considered as a treatment option. However, as the specificity of MR for detection of breast malignancy still lags behind sensitivity, MRI biopsy capability is essential to allow assessment of MRI-only detected lesions.
Disclosures
No financial or ethical disclosures.
| References | ▴Top |
- Lim HS, Jeong SJ, Lee JS, Park MH, Kim JW, Shin SS, Park JG, et al. Paget disease of the breast: mammographic, US, and MR imaging findings with pathologic correlation. Radiographics. 2011;31(7):1973-1987.
pubmed doi - Echevarria JJ, Lopez-Ruiz JA, Martin D, Imaz I, Martin M. Usefulness of MRI in detecting occult breast cancer associated with Paget's disease of the nipple-areolar complex. Br J Radiol. 2004;77(924):1036-1039.
pubmed doi - Kim HS, Seok JH, Cha ES, Kang BJ, Kim HH, Seo YJ. Significance of nipple enhancement of Paget's disease in contrast enhanced breast MRI. Arch Gynecol Obstet. 2010;282(2):157-162.
pubmed doi - Morrogh M, Morris EA, Liberman L, Van Zee K, Cody HS, 3rd, King TA. MRI identifies otherwise occult disease in select patients with Paget disease of the nipple. J Am Coll Surg. 2008;206(2):316-321.
pubmed doi - Frei KA, Bonel HM, Pelte MF, Hylton NM, Kinkel K. Paget disease of the breast: findings at magnetic resonance imaging and histopathologic correlation. Invest Radiol. 2005;40(6):363-367.
pubmed doi - Jansen SA, Shimauchi A, Zak L, Fan X, Karczmar GS, Newstead GM. The diverse pathology and kinetics of mass, nonmass, and focus enhancement on MR imaging of the breast. J Magn Reson Imaging. 2011;33(6):1382-1389.
pubmed doi - Baltzer PA, Benndorf M, Dietzel M, Gajda M, Runnebaum IB, Kaiser WA. False-positive findings at contrast-enhanced breast MRI: a BI-RADS descriptor study. AJR Am J Roentgenol. 2010;194(6):1658-1663.
pubmed doi - Siziopikou KP, Jokich P, Cobleigh M. Pathologic findings in MRI-guided needle core biopsies of the breast in patients with newly diagnosed breast cancer. Int J Breast Cancer. 2011;2011:613285.
pubmed - Kuhl CK, Schrading S, Bieling HB, Wardelmann E, Leutner CC, Koenig R, Kuhn W, et al. MRI for diagnosis of pure ductal carcinoma in situ: a prospective observational study. Lancet. 2007;370(9586):485-492.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
